Case Report - (2022) Volume 7, Issue 1
Lichen planopilaris of the external auditory canal-a case report with a review of literature
2Department of Dermatology and Venereology, Military Medical Academy, Sofia, Bulgaria
Received Date: Dec 17, 2021 / Accepted Date: Dec 23, 2021 / Published Date: Jan 03, 2022
Copyright: ©Copyright: ©2022: Valentina Broshtilova, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Gergi Kukushev, Valentina Broshtilova (2022) Lichen planopilaris of the external auditory canal-a case report with a review of literature. Journal of Clinical Review & Case Reports 7(1):791-793.
Abstract
A 73-year-old female with citactricial alopecia of the fronto-parietal zone of the scalp due to a pro-longed history of lichen plano-pilaris presented with a progressive hearing loss and obstruction of the left auditory canal as well as ring stenosis and mild purulent discharge of the right auditory canal. Histopatologically, the ear involvement was verified in the lichen planus inflammatory spectrum. Complete medial external auditory canal skin elevation of the left ear and excision of the ring stenosis on the right side were performed in association with appropriate systemic immunomodulating therapy. The therapeutic surgical and pathogenetic modalities are reviewed to highlight the possible management of this extremely rare lichen planus complication.
Keywords
Follicular Lichen Planus, External Auditory Canal
Introduction
Lichen planus is a chronic inflammatory disease which affects skin and mucosal membranes. It encompasses a versatile clinical manifestation that depends on the affected localizations [1]. The follicular variant of the disease irreversibly destruct the hair follicular stem cells to cause permanent loss of regenerative capacity and cicatricial alopecia [2]. A T-cytotoxic mediated immune response directed by infectious (HBV or HCV), toxic (drug-induced), metabolic (hyperglycemia, dyslipidemia, etc.) and haptenic antigens on the keratinocytic surface enhance their apoptosis and consecutive epidermal dysfunction [3]. Less than 1% of the world population present some forms of lichen planus, hence, follicular form is considered one of the most anecdotal [4].
Herein, a very rare case of lichen plano-pilaris affecting the auditory external canals is presented.
Case Report
A -73-year-old female was admitted to the ORL department with a history of progressive hearing loss on the left side, and a purulent discharge from the right ear over the last 3 years. Pain and intensive pruritus worsened the clinical picture two weeks prior the hospitalization. The anamnesis revealed that the patient was affected by lichen plano-pilaris with 15-year duration. The condition was treated with intralesional corticosteroids and oral hydroxychloroquine 200 mg daily for 7 year period and a clinical remission was obtained in the last 2 years. No other relevant comorbidies and concomitant treatment modalities were reported.
The dermatological examination showed areas of citactricial alopecia with a diameter of 5 cm in the fronto-parietal zone of the scalp. The skin was atrophic, with total loss of follicular ostia. The periphery of the scarring lesions showed no signs of active inflammation erythema, pityriasiform desquamation and perifollicular plugging.
The otomicroscopy and the otoendoscopy showed totally stenotic left external auditory canal (EAC) and ring stenosis on the right EAC in the bony/cartilage portion (Figure 1) with mild purulent discharge. Tympanic membrane was visible only right side with no pathological alterations. Tonal audiometry revealed presbyacusis both sides and conductive hearing loss on the left ear.
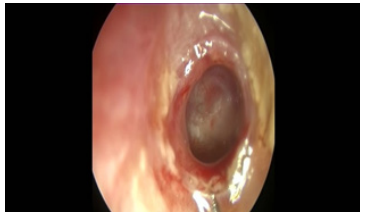
Figure 1: Ring stenosis on the right EAC in the bony/cartilage portion.
A computed tomography of the temporal bone (Figure 2) revealed an important amount of isodense soft tissue occupying the left EAC and discrete stenosis on the right side. Middle ear and mastoid process were both sides intact.
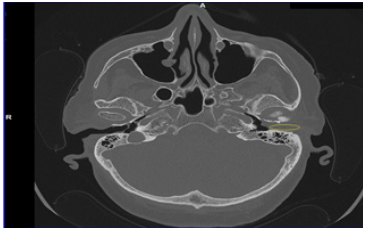
Figure 2: Computed tomography of the temporal bone.
A surgical intervention was indicated. After sterile preparation of the left external ear canal first a left side transcanal approach was chosen. The stenosis was about 4 mm, covering the tympanic membrane and a large portion of the EAC from the cartilaginous to bony part. It was totally excised. The edges of the wound were infiltrated with corticosteroid to avoid further stenosis. Antibiotic (Levofloxacin) with dexamethasone dressing was inserted into the left EAC. Similar procedure was performed in the right side.
The histopatological analysis showed hyperkeratosis, atrophic epidermis, vacuolar degeneration of the basal keratinocytic layer with plenty of ovoid bodies intermingled in the dense lichenoid lympho-plasmocytic inflammatory infiltrate in the papillary dermis. These findings were consistent with lichen planus (Figure 3).
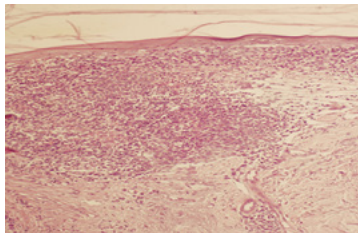
Figure 3: Hyperkeratosis, atrophic epidermis, dense lichenoid lympho-plasmocytic inflammatory infiltrate to cause vacuolar degeneration and obscuration of the dermal-epidermal junction (H&E,x200).
Topical corticosteroid otologic eardrops were introduced for two weeks together with per oral pathogenetic therapy with 200 mg hydroxychloroquine on a continuing everyday basis for 6 months. On the follow up visit at the end of the third month, the itch and ear pain were un-noticeable and there were no otoscopical signs of external auditory canal inflammation. Only the bilateral presbyacusis persisted.
Discussion
Otic lichen planus is clinically manifestated by a conductive hearing loss, running ear, pruritus, pain, tinnitus, and bleeding [5]. It is extremely rare and probably under-diagnosed. To date, there are only 25 cases reported worldwide [6].
Recently published analysis shows female preponderance (4:1) and a mean age of onset 63 years. Most of the patients have a history of pre-existing lichen planus of unknown localization (skin, mucosal or follicular) with duration of the concomitant otic symptoms ranging from 14 years to 6 months. Otological involvement is monolateral in half of the cases. The clinical diagnosis is suspected, based on conductive hearing loss and auditory canal stenosis and verified by histological examination [7].
Most of the cases were managed with topical pathogenetic therapy-calcineurin inhibitors and corticosteroids. One case was treated with oral prednisolone (1 mg/kg/day) with no sufficient effect and another one was put on a short-course of acitretine with temporary clinical improvement. Most scientific groups prefer topical corticosteroid therapy, given for 2-3 weeks every month [6,7].
A conductive or mixed hearing loss is the most common symptom due to the EAC stenosis in patients with otic LP. No therapeutic strategies have been reported to date, probably due to the scarcity of the scientific observations. A few surgical approaches have been introduced with controversial outcomes [8]. The use of conventional hearing aids is beneficial, especially if the EAC is not totally occluded and an earmold can be fitted [9]. Upon applying such devices, however, a specialist should always consider the risk of provoking a Koebner phenomenon (a relapse of active LP inflammation induced by mechanical trauma and injury of the EAC). Therefore, non-invasive anti-hearing loss techniques such as ADHEAR® (MED-EL®) should be referred as most appropriate preventive measures.
Despite the precise surgical treatment, a pathogenetic argumentated modality is of utmost need, since even adequate ventilation cannot prevent the fibrotic stenotic inflammation due to T-cytotoxic infiltration and vacuolar degeneration of the basal membrane. In this respect, topical corticosteroids or calcineurin inhibitors alone or in association with systemic immune suppressors such as hydroxychloroquine should be considered.
Our patient has involvement of the external auditory canals in the clinical context of follicular lichen planus. To note, the scarring alopecia was long-standing with no signs of recurrence and inflammatory activation. However, the risk of chronification and permanent otic dysfunction motivated the introduction of hydroxychloroquine as effective prevention of T-cell mediated immune aggression of the bulge zone of the tragi, which we believe, are the targets of induction and persistence of the autoinflammatory process.
Conclusion
A very rare otic localization of lichen planus is herein reported. The extra-ordinary findings are even more peculiar since they appear in the clinical context of follicular lichen planus. We suggest the hypothesis that T-cell mediated cytotic effect on the proliferating zone of the follicular units in the external auditory canals cause permanent hair loss and chronic fibrotic obliteration. Therefore, more complex pathogenetic therapy, combining topical corticosteroid modalities and per oral disease-modifing medications, is considered necessary and more effective. The rarity of the EAC involvement in lichen planus alerts further investigation, multi-disciplinary approach and more precise medical expertise to highlight the proper pathogenetic mechanisms and future management strategies.
Conflict of Interest Statement
No conflict of interests.
Financial Disclosures
No financial disclosure.
References
1. Boch K, Langan EA, Kridin K, Zillikens D, Ludwig RJ and Bieber K (2021) Lichen Planus. Fron Med 8: 737- 813.
2. Wagner G, Rose C, Sachse MM (2013) Clinical variants of lichen planus. J Dtsch Dermatol Ges 11: 309-319.
3. Diop A, Ly F, Ndiaye MT, Seck B, El Omari A, Diouf A, et al. (2020) Epidemiology, clinical features, and associated factors in 78 cases of lichen planus on black skin. Int J Dermatol 59:137-142.
4. Pavlovsky L, Israeli M, Sagy E, Berg AL, David M, Shemer A, et al. (2015) Lichen planopilaris is associated with HLA DRB1*11 and DQB1*03 alleles. Acta Derm Venereol 95: 177-180.
5. Martin L, Moriniere S, Machet MC, Robier A, Vaillant L (1998) Bilateral conductive deafness related to erosive lichen planus. J Laryngol Otol 112: 365-366.
6. Kosec A, Kostic M, Ajduk J, Ries M (2019) Hypertrophic recurring lichen planus of the external auditory canal. Eur Ann Otorhinolaryngol Head Neck Dis 136: 123-126.
7. Sartori-Valinotti JC, Bruce AJ, Krotova Khan Y, Beatty CW (2013) A 10-year review of otic lichen planus: the Mayo Clinic experience. JAMA Dermatol 149: 1082-1086
8. Hopsu E, Pitkaranta A (2007) Idiopathic, inflammatory, medial meatal, fibrotising otitis presenting with lichen planus. J Laryngol Otol 121: 796-799.
9. Lazzerini F, Bruschini L, Berrettini S, De Vito A, Forli F (2020) Lichen planus of the external auditory canal: treatment options ans review of literature. Clin Case Rep 8: 2017-2020.