Case Report - (2025) Volume 10, Issue 1
Electric Chaos: A Challenging Case of Atrial Fibrillation in Wolff-Parkinson-White Syndrome
Received Date: Mar 04, 2025 / Accepted Date: Apr 03, 2025 / Published Date: Apr 10, 2025
Copyright: ©©2025 Ahmad Murtaza Anwar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Anwar, A. M. (2025). Electric Chaos: A Challenging Case of Atrial Fibrillation in Wolff-Parkinson-White Syndrome. Cardio Open, 10(1), 01-03.
Abstract
Atrial fibrillation involves multiple interatrial reentry circuits and the presence of accessory pathways congenitally between atrium and ventricle makes the condition even worse. Common triggering factors include rapidly discharging atrial foci, or atrial flutter. The common presenting features include palpitations, shortness of breath, and sweating and if not managed early may lead to syncope, ventricular fibrillation, and even death. A case of a young patient having WPW syndrome is being presented here to highlight the importance of early interpretation of electrocardiographic findings for proper treatment and management of the patient.
Keywords
Atrial Fibrillation (AF), WPW-Syndrome, Wolf-Parkinson-White Syndrome, Palpitations, ECG, Syncope, Delta Waves
Introduction
Atrial fibrillation (AF) involves multiple interatrial reentry circuits and the presence of accessory pathways congenitally between atrium and ventricle (known as Wolff-Parkinson-White Syndrome) makes the condition even worse. Common triggering factors include rapidly discharging atrial foci, atrial flutter or atrial tachycardia into fibrillation [1]. The common presenting features include palpitations, shortness of breath, and sweating and if not managed early may lead to syncope, ventricular fibrillation, and even death [2]. Correct and early interpretation of electrocardiographic (ECG) findings is important for proper treatment and management of the patient. Worldwide, atrial fibrillation is the leading cause of sustained arrhythmia affecting more than 1 % of the world’s population [3]. We present a case of a patient with hemodynamically stable atrial fibrillation with WPW syndrome and remarkable recovery following prompt emergency treatment.
Case History
A 31-year-old man was presented to cardiac emergency with complaints of palpitations, sweating, and dizziness for 2 hours. He has no previous history of heart disease, thyroid disorder, hypertension, and diabetes mellitus. At the time of presentation, his blood pressure was 90/60 mmHg and oxygen saturation in room air was 95%. Physical examination revealed a Glasgow Coma Scale of 15/15, while inspection revealed cold and clammy skin. The cardiac auscultation revealed an abnormally fast heart rate (180-200 beats per minute). An electrocardiogram (ECG) was immediately obtained, Figure 1.
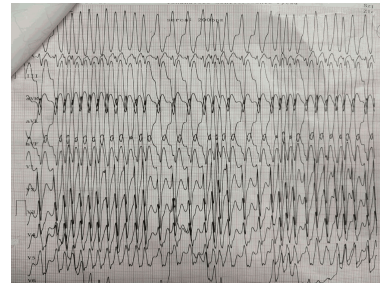
Figure 1: 12 Lead Electrocardiographic (ECG) Recording of a Patient Showing Atrial Fibrillation (AF) with Wolff-Parkinson-White (WPW) Syndrome at the Time of Presentation at Cardiac Emergency
ECG showed irregularly irregular rhythm with broad QRS complexes and delta waves which led to the diagnosis of fast ventricular rate Atrial Fibrillation with WPW syndrome. As the patient was hemodynamically stable, intravenous procainamide was administered, and the patient was kept for close monitoring at the critical cardiac care unit (CCU). After half an hour, a second ECG was obtained which revealed fast ventricular rate has settled, Figure 2. Next day, the patient was taken to the catheterization lab, and the accessory pathway was successfully removed by catheter ablation.
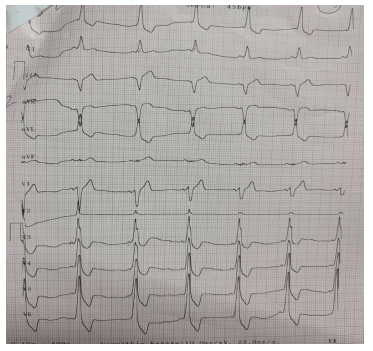
Figure 2: 12 Lead Electrocardiographic (ECG) Recording of the Patient Showing Atrial Fibrillation (AF) with Wolff-Parkinson-White (WPW) Syndrome after Administration of Intravenous Procainamide
Differential Diagnosis
Atrial fibrillation in WPW syndrome and ventricular tachycardia are two key differential diagnoses for this patient.
Outcome & Follow-Up
The patient was discharged the next day with anticoagulation medications. At one week’s follow-up after discharge, his vital signs were normal, and he reported no complaints
Discussion
The incidence of AF is much greater in patients with WPW syndrome than in a similar group of patients without accessory pathway [2]. Therefore, it can be inferred that accessory pathways have a key role in atrial fibrillation genesis. Sharma et al. showed that patients who had undergone an ablation of the accessory pathway demonstrated significantly fewer incidences of atrial fibrillation. The diagnosis is made by classic electrocardiographic (ECG) findings that include an irregularly irregular rhythm with short PR interval and broad QRS complex with delta wave (slurring upstroke) [4]. The patient, previously having no comorbidities, presented with palpitations and dizziness. ECG findings can be easily confused with ventricular tachycardia (VT) by a person who has not a sound knowledge of electrocardiography. Early diagnosis of the patient’s condition is important as delay in treatment can lead to complications like ventricular fibrillation and even death.
Page et al. gave separate guidelines for both hemodynamically stable and unstable patients. If the patient is hemodynamically stable, class 1A anti-arrhythmic drugs are the preferred option, however, if the patient is hemodynamically unstable then cardioversion is preferred, followed by catheter ablation [5]. The uniqueness of this report is that the patient has not experienced any cardiac symptoms before and at the time of presentation, he was stable. Smoking, caffeine, alcohol, antihistamines, and cocaine should be avoided by patients who have accessory pathways in their hearts as these substances can lead to aggravation of their condition.
Acknowledgement
The author would like to express his gratitude to the medical team at Kashmir Institute of Cardiology Mirpur for treating this patient.
Learning Objective
The case report reinforces the fact that patients’ lives can be saved through early diagnosis and treatment. Every medical facility should make basic knowledge of ECG and ATLS mandatory for all the health workers working in the emergency department.
Consent
A written informed consent was obtained from the patient for the publication of this case report.
References
1. Scheinman, M. M. (2000). Mechanisms of atrial fibrillation: is a cure at hand? Journal of the American College of Cardiology, 35(6), 1687-1692.
2. Pietersen, A. H., Andersen, E. D., & Sandøe, E. (1992). Atrial fibrillation in the Wolff-Parkinson-White syndrome. The American journal of cardiology, 70(5), A38-A43.
3. Chugh, S. S., Havmoeller, R., Narayanan, K., Singh, D., Rienstra, M., Benjamin, E. J., ... & Murray, C. J. (2014). Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation, 129(8), 837-847.
4. Bhatia, A., Sra, J., & Akhtar, M. (2016). Preexcitation syndromes. Current problems in cardiology, 41(3), 99-137.
5. Page, R. L., Joglar, J. A., Caldwell, M. A., Calkins, H., Conti, J. B., Deal, B. J., ... & Al-Khatib, S. M. (2016). 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 67(13), e27-e115



