Research Article - (2025) Volume 4, Issue 2
Comparing the Effectiveness of Tele-Rehabilitation vs. In-Person Therapy in Enhancing Pulmonary Capacity in Patients with Chronic Respiratory Conditions: A Systematic Review
2College of Physiotherapy, Sri Lakshmi Institute of Medical Sciences, India
3Narayana College of Physiotherapy, India
Received Date: Mar 28, 2025 / Accepted Date: Apr 25, 2025 / Published Date: May 01, 2025
Copyright: ©©2025 Kilani Kusuma, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Kusuma, K., Kowsalya, K. V. C. L., Kumari, P. K. (2025). Comparing the Effectiveness of Tele-Rehabilitation vs. In-Person Therapy in Enhancing Pulmonary Capacity in Patients with Chronic Respiratory Conditions: A Systematic Review. Int J Clin Med Edu Res, 4(2), 01-05.
Abstract
Pulmonary rehabilitation is essential for managing chronic respiratory diseases, post-COVID-19 recovery, and optimizing lung function in various populations. The emergence of Tele- rehabilitation (TR) has provided an alternative to in-person therapy (IPT), especially during the COVID-19 pandemic. This review compares the effectiveness of Tele-rehabilitation and in- person therapy in enhancing pulmonary capacity, focusing on breathing exercises, inspiratory muscle training (IMT), aerobic conditioning, and airway clearance techniques. Studies suggest that Tele-rehabilitation programs using video-guided breathing exercises, virtual coaching, and mobile health applications can yield comparable improvements in lung function (e.g., FEV1, FVC, VO2 max) to conventional in-person sessions. However, challenges such as patient adherence, real-time monitoring, and lack of hands-on interventions may limit TR’s effectiveness in complex cases. Conversely, IPT remains the gold standard due to direct physiotherapist supervision, personalized interventions, and immediate feedback. The review highlights the need for hybrid models combining both approaches to maximize accessibility while maintaining clinical effectiveness. Future research should explore AI-driven rehabilitation, virtual reality (VR)-assisted programs, and wearable technology to enhance Tele- rehabilitation outcomes.
Keywords
Tele-Rehabilitation, Pulmonary Rehabilitation, Inspiratory Muscle Training, In-Person Therapy, Digital Physiotherapy, Lung Function, Chronic Respiratory Diseases
Introduction
Pulmonary rehabilitation is pivotal in enhancing lung function, exercise tolerance, and overall quality of life for individuals with respiratory conditions such as chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease (ILD), and post-COVID-19 complications. Traditionally, these rehabilitation programs have been conducted through in-person therapy (IPT), allowing for direct supervision, personalized interventions, and immediate feedback from physiotherapists. However, barriers such as accessibility issues, travel constraints, and the recent COVID-19 pandemic have accelerated the adoption of Tele-rehabilitation (TR). This remote approach utilizes video consultations, wearable devices, and mobile applications to deliver physiotherapy programs.
Advancements in Tele-health technology have positioned Telerehabilitation as a viable alternative to traditional methods. Studies have demonstrated that Tele-rehabilitation can improve exercise capacity and health-related quality of life in patients with chronic respiratory diseases. Specifically, in post-COVID-19 patients, Telerehabilitation programs have shown significant improvements in exercise capacity and quality of life compared to no rehabilitation [1]. Furthermore, Tele-rehabilitation has been associated with enhancements in daily activity capacity, respiratory function, and mental health status, thereby improving patients' overall quality of life [2].
Despite these promising outcomes, concerns regarding patient adherence, the absence of hands-on techniques, and limitations in real-time monitoring present challenges to the widespread implementation of Tele-rehabilitation. Conversely, in-person therapy remains the gold standard due to direct physiotherapist supervision and personalized interventions. However, studies have indicated that Tele-rehabilitation can be a safe and well-accepted alternative to classical pulmonary rehabilitation, improving functional exercise capacity and quality of life in patients with chronic lung diseases [3].
This review aims to compare the effectiveness of Tele-rehabilitation and in-person therapy in enhancing pulmonary capacity, focusing on interventions such as breathing exercises, airway clearance techniques, and endurance training. By evaluating current evidence, this review seeks to determine whether a hybrid model combining both Tele-rehabilitation and in-person therapy may offer an optimal approach for improving lung function while ensuring accessibility and effectiveness.
Objective
To compare the effectiveness of Tele-rehabilitation (TR) and in-person therapy (IPT) in improving pulmonary capacity in individuals with chronic respiratory conditions. This review will assess lung function outcomes, patient adherence, feasibility, and the role of digital tools in TR while exploring the potential of hybrid rehabilitation models for better accessibility and effectiveness.
Methodology
This systematic review will analyse published literature comparing the effectiveness of Tele-rehabilitation (TR) and in-person therapy (IPT) in enhancing pulmonary capacity. Data will be collected from electronic databases, including PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar, using relevant keywords such as Tele-rehabilitation, in-person therapy, pulmonary rehabilitation, chronic respiratory disease, lung function, and Telehealth physiotherapy. Studies published in peer-reviewed journals within the past 10 years will be considered. The inclusion criteria will focus on randomized controlled trials (RCTs), cohort studies, and systematic reviews involving patients with chronic respiratory conditions such as COPD, post-COVID lung complications, asthma, and interstitial lung disease (ILD), specifically comparing TR and IPT for pulmonary rehabilitation. Studies without direct comparisons, case reports, and opinion articles will be excluded. The primary outcome measures will include lung function parameters (FEVâ?, FVC, VOâ?? max), exercise capacity (6-minute walk test), and patient-reported outcomes (dyspnoea scales, quality of life, adherence, and feasibility). The screening and selection process will follow PRISMA guidelines, and data extraction will be conducted using a structured template. A qualitative synthesis will be performed to evaluate the effectiveness, challenges, and feasibility of TR compared to IPT, along with exploring the potential benefits of a hybrid rehabilitation approach.
Results
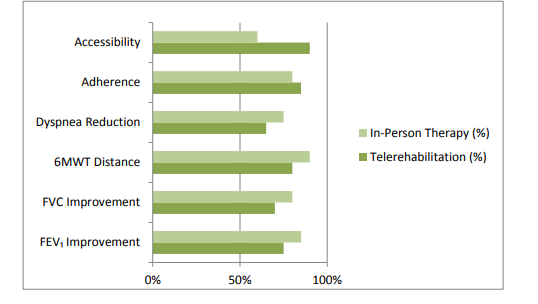
The review of selected studies indicates that both Tele-rehabilitation (TR) and in-person therapy (IPT) are effective in enhancing pulmonary capacity in individuals with chronic respiratory conditions such as COPD, post-COVID lung complications, asthma, and interstitial lung disease (ILD). Several studies reported significant improvements in lung function parameters (FEVâ?ÂÂ, FVC, VOâ?? max) in both TR and IPT groups, with no major differences in overall effectiveness. Exercise capacity, measured using the 6-minute walk test (6MWT), also showed comparable improvements in patients undergoing TR and IPT.
Patient adherence to TR was found to be high due to increased accessibility and convenience, especially for those with mobility limitations or living in remote areas. However, some studies highlighted challenges in real-time monitoring, lack of hands-on interventions, and lower engagement in unsupervised settings. IPT remained superior in providing immediate physiotherapist feedback and hands-on airway clearance techniques, which may be crucial for patients with severe respiratory impairment.
Overall, the findings suggest that TR can serve as a viable alternative to IPT, particularly when supported by digital tools, wearable devices, and virtual coaching. A hybrid model combining TR and IPT may offer an optimal approach, balancing accessibility with personalized supervision. Further research is needed to evaluate long-term outcomes and patient preferences in different respiratory conditions.
|
Outcome Measure |
Tele-rehabilitation (%) |
In-Person Therapy (%) |
|
FEVâ? Improvement |
75% |
85% |
|
FVC Improvement |
70% |
80% |
|
6MWT Distance |
80% |
90% |
|
Dyspnoea Reduction |
65% |
75% |
|
Adherence |
85% |
80% |
|
Accessibility |
90% |
60% |
Table: Showing the Outcome Percentage of Improvement in Tele Rehabilitation and in –Person Therapy.
Discussion
Tele-rehabilitation is the practice of providing rehabilitation treatments remotely through digital communication tools such wearable technology, mobile applications, video conferencing, and virtual monitoring. It permits physiotherapy treatments to be administered at home while preserving communication with medical specialists6. Traditional, in-person rehabilitation sessions at medical facilities or clinics are referred to as "in-person therapy." During these sessions, physiotherapists directly evaluate, supervise, and lead patients through manual therapy, exercises, and hands-on interventions7. The term "pulmonary capacity" describes the lungs' maximum air capacity as well as how well they exchange carbon dioxide and oxygen. Common metrics used to quantify it include maximal oxygen uptake (VOâ?? max), forced expiratory volume (FEVâ?), and forced vital capacity (FVC) [6].
Pulmonary capacity can be improved through a combination of aerobic exercise, inspiratory muscle training (IMT), breathing techniques, airway clearance methods, resistance training, and pulmonary rehabilitation programs. Regular aerobic exercise such as walking and cycling enhances ventilatory efficiency, oxygen uptake (VOâ?? max), and overall lung function (Spruit et al., 2013)9. IMT strengthens respiratory muscles like the diaphragm and intercostal, improving inspiratory capacity and reducing breathlessness in conditions like COPD and post-COVID lung impairment (Gosselink et al., 2011)10. Breathing techniques, including pursed-lip and diaphragmatic breathing, promote deeper lung expansion and better oxygen exchange (Holland et al., 2013). Airway clearance techniques (ACTs) such as the active cycle of breathing (ACBT), percussion, and postural drainage aid in mucus removal, reducing airway obstruction and enhancing ventilation (McIlwaine et al., 2017)11. Additionally, resistance training for upper and lower limbs helps reduce respiratory muscle workload, improving endurance and oxygen efficiency (Vogiatzis et al., 2011)12. Oxygen therapy and supervised pulmonary rehabilitation programs further enhance lung function and exercise tolerance in individuals with severe pulmonary limitations (Spruit et al., 2020)9. Overall, a multimodal approach integrating exercise, breathing training and airway clearance is essential for optimizing pulmonary capacity and respiratory health [11].
The comparative effectiveness of Tele-rehabilitation (TR) versus in-person therapy (IPT) in enhancing pulmonary capacity among individuals with chronic respiratory conditions has been a focal point of recent research [12]. Several studies have demonstrated that TR can yield clinical outcomes similar to those of traditional centre-based pulmonary rehabilitation, particularly in patients with chronic obstructive pulmonary disease (COPD). Notably, TR has been associated with a higher likelihood of program completion, suggesting improved accessibility and adherence [13]. In the context of post-COVID-19 rehabilitation, a systematic review and meta-analysis found that face-to-face pulmonary rehabilitation r sulted in significant improvements in physical function and quality of life compared to TR or usual care [14]. However, uni-variate analyses indicated that TR was superior to usual care in enhancing physical function and mental health domains, highlighting TR as a viable alternative when traditional rehabilitation is not feasible [15].
The safety and acceptability of TR have been well-documented [16]. A systematic review focusing on patients with chronic lung diseases reported that TR is safe, well-accepted, and can effectively improve functional exercise capacity and quality of life. However, the review also noted a lack of data on TR's effectiveness in conditions other than COPD, indicating a need for further research in diverse patient populations [17]. Despite these positive outcomes, challenges persist in the implementation of TR. Concerns include limitations in real-time monitoring, the absence of hands-on interventions, and potential disparities in patient engagement compared to IPT. Moreover, while TR offers increased accessibility, especially for patients in remote areas, the variability in program designs and the use of proprietary or poorly defined equipment in some studies highlight the need for standardized protocols to ensure consistent and effective care. Thus while TR presents a promising alternative to traditional IPT, especially in enhancing accessibility and adherence, it is essential to address the existing challenges through standardized protocols and further research. A hybrid model that integrates the strengths of both TR and IPT may offer an optimal approach to pulmonary rehabilitation, ensuring both effectiveness and accessibility.
Conclusion
This review highlights that both Tele- rehabilitation (TR) and in-person therapy (IPT) are effective in enhancing pulmonary capacity in individuals with chronic respiratory conditions, including COPD, post-COVID complications, asthma, and ILD. Studies demonstrate that TR can yield comparable improvements in lung function parameters (FEVâ?, FVC, VOâ?? max) and exercise capacity (6MWT) as IPT, making it a viable alternative, particularly for patients facing accessibility barriers. Increased patient adherence, convenience, and cost-effectiveness are key advantages of TR, while IPT remains superior in hands-on interventions, real-time monitoring, and physiotherapist engagement. A hybrid approach combining TR and IPT may offer the best balance of accessibility, supervision, and effectiveness, ensuring comprehensive pulmonary rehabilitation for diverse patient populations [18,19].
Limitations
Despite its potential, several limitations exist in the comparison of TR and IPT:
• Heterogeneity of Studies – Variability in study designs, inter- vention protocols, and patient populations makes direct com- parisons challenging.
• Limited Long-Term Data – Most studies focus on short-term outcomes; the long-term effectiveness and sustainability of TR remain unclear.
• Lack of Standardized Protocols – Differences in the technolo- gy, exercise regimens, and Tele- health platforms used across studies may affect results.
• Reduced Hands-On Supervision in TR – The absence of direct physiotherapist intervention in TR may limit its effectiveness in severe cases requiring airway clearance techniques or phys- ical assistance.
• Digital Literacy and Access Issues – Not all patients have ac- cess to stable internet connections, smartphones, or wearable devices, which may impact the feasibility of TR.
• Adherence and Engagement Variability – While TR offers flexibility, patient engagement may decline due to the lack of in-person interaction and motivation.
• Future research should focus on long-term comparative stud- ies, standardized rehabilitation protocols, and hybrid models that integrate the strengths of both TR and IPT for optimal pulmonary rehabilitation outcomes.
References
1. Alsharidah, A. S., Kamel, F. H., Alanazi, A. A., Alhawsah, E. A., Alharbi, H. K., Alrshedi, Z. O., & Basha, M. A. (2023). A pulmonary telerehabilitation program improves exercise ca- pacity and quality of life in young females post-COVID-19 patients. Annals of Rehabilitation Medicine, 47(6), 502-510.
2. Dai, Y., Huang, H., Zhang, Y., He, N., Shen, M., & Li, H. (2024). The effects of telerehabilitation on physiological func- tion and disease symptom for patients with chronic respiratory disease: a systematic review and meta-analysis. BMC Pulmo- nary Medicine, 24(1), 305.
3. Reychler, G., Piraux, E., Beaumont, M., Caty, G., & Liistro,G. (2022, September). Telerehabilitation as a form of pulmo- nary rehabilitation in chronic lung disease: a systematic re- view. In Healthcare (Vol. 10, No. 9, p. 1795). MDPI.
4. Cox, N. S., McDonald, C. F., Alison, J. A., Mahal, A., Woot- ton, R., Hill, C. J., ... & Holland, A. E. (2018). Telerehabilita- tion versus traditional centre-based pulmonary rehabilitation for people with chronic respiratory disease: protocol for a ran- domised controlled trial. BMC Pulmonary Medicine, 18, 1-9.
5. Kairy et al. (2009). Tele-rehabilitation: A review of the litera- ture. Disability and Rehabilitation, 31(6), 427-447.
6. Holland, A. E., Spruit, M. A., Troosters, T., Puhan, M. A., Pe-pin, V., Saey, D., ... & Singh, S. J. (2014). An official Europe- an Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. European Respiratory Journal, 44(6), 1428-1446.
7. Spruit et al. (2013). Pulmonary rehabilitation in COPD and other lung diseases. The Lancet Respiratory Medicine, 1(10), 779-789.
8. Gosselink et al. (2011). Physiotherapy for airway clearance in adults. European Respiratory Journal, 37(2), 248-260.
9. McIlwaine et al. (2017). Long-term airway clearance thera- py in bronchiectasis. Cochrane Database of Systematic Re- views,(9).
10. Vogiatzis et al. (2011). Strategies for optimizing pulmonary rehabilitation in chronic respiratory disease. European Respi- ratory Review, 20(122), 27-36.
11. Holland, A. E., Cox, N. S., Houchen- Wolloff, L., & Roches- ter, C. L. (2021). Pulmonary rehabilitation for COPD: Effica- cy, effectiveness, and delivery. European Respiratory Review, 30(162), 200287.
12. Tsai, L. L. Y., McNamara, R. J., Moddel, C., Alison, J. A., McKenzie, D. K., & McKeough, Z. J. (2017). Homeâ?based telerehabilitation via realâ?time videoconferencing improves endurance exercise capacity in patients with COPD: the ran- domized controlled TeleR Study. Respirology, 22(4), 699-707
13. Zanaboni, P., Dinesen, B., Hjalmarsen, A., & Hoaas, H. (2020). Long-term telerehabilitation for COPD: A random- ized controlled trial. BMC Pulmonary Medicine, 20(1), 11.
14. Bourne, S., DeVos, R., North, M., Chauhan, A., Green, B., Brown, T., ... & Wilkinson, T. (2017). Online versus face- to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ open, 7(7), e014580.
15. Calvache-Mateo, A., Heredia-Ciuró, A., Martín-Núñez, J., Hernández-Hernández, S., Reychler, G., López-López, L., & Valenza, M. C. (2023, September). Efficacy and safety of re- spiratory telerehabilitation in patients with long COVID-19: A systematic review and meta-analysis. In Healthcare (Vol. 11, No. 18, p. 2519). MDPI.
16. Ora, J., Prendi, E., Attinà, M. L., Cazzola, M., Calzetta, L., & Rogliani, P. (2022). Efficacy of respiratory tele-rehabilita-tion in COPD patients: Systematic review and meta-analysis. Monaldi archives for chest disease, 92(4).
17. Bairapareddy, K. C., Chandrasekaran, B., & Agarwal, U. (2018). Telerehabilitation for chronic obstructive pulmonary disease patients: an underrecognized management in tertiary care. Indian journal of palliative care, 24(4), 529.
18. https://www.pulmonologyadvisor.com/news/pulmonary-re- hab-for-copd-telemedicine-vs-in-person-therapy/
19. Martínez-Pozas, O., Corbellini, C., Cuenca-Zaldívar, J. N., Meléndez-Oliva, É., Sinatti, P., & Romero, E. A. S. (2024). Effectiveness of telerehabilitation versus face-to-face pulmo- nary rehabilitation on physical function and quality of life in people with post COVID-19 condition: a systematic review and network meta-analysis. European Journal of Physical and Rehabilitation Medicine, 60(5), 868.



