Case Report - (2022) Volume 7, Issue 8
A Rare case of amyands hernia managed with laparoscopic repair
2Teaching Hospital Kurunegala, Sri Lanka
Received Date: Jun 30, 2022 / Accepted Date: Aug 03, 2022 / Published Date: Aug 16, 2022
Copyright: ©Copyright: ©2022: Sayanthan B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Sayanthan B, Sajeevan P and Dhadchayini R (2022) A Rare case of amyand’s hernia managed with laparoscopic repair. Journal of Clinical Review & Case Reports 7(8):107-109.
Abstract
Amyand’s hernia is defined as when the appendix is trapped within an inguinal hernia. Although the incidence of Amyand’s hernia is rare, the appendix may become incarcerated within Amyand’s hernia and lead to further complications such as mechanical obstruction, strangulation, necrosis, perforation and catastrophic peritonitis. The aim of this paper is to provide insight into the diagnosis and treatment of Amyand’s hernia by describing the familiarization of the incarcerated appendixes within hernias in order to ensure potential successful surgical outcomes and avoid unexpected surgical complications.
Keywords
Amyand’s hernia, Incarcerated Hernia, Laparoscopic Exploration.
Introduction
The protrusion of abdominal contents through the inguinal canal is termed as inguinal hernia. A content of inguinal canal varies; usual contents are bowel and omentum. But it varies from liver, bladder, Merkel’s diverticulum, uterus and fallopian tube. When the appendix is trapped within an inguinal hernia it defined as Amyand’s hernia. It is rare form of inguinal hernia, which occurs up to 1% [1]. The appendix may inflamed or non-inflamed or incarcerated and incidence of appendicitis in Amyand’s hernia only around 0.1%. Although the Amyand’s hernia is rare, the appendix may become incarcerated within Amyand’s hernia and lead to further complications such as mechanical obstruction, strangulation, necrosis, perforation and catastrophic peritonitis [2,3]. The appendix incarceration more commonly happens within inguinal and femoral hernias (De Garengeot’s hernia) though it is unlikely to extend in the cases of incisional and umbilical hernias. It has been reported that incarcerated appendix in a variety of ventral abdominal and inguinal locations, however, there is a diagnostic challenge on its indistinct clinical presentation. The precise differential diagnosis is quite challenging for the treating clinicians due to the lack of different clinical signs and symptoms as well as the vague radiological diagnostic clinical features. For instance, incarcerated appendix is quite often misdiagnosed as a strangulated hernia [1]. The finding of Amyand’s hernia occurs incidentally during surgery thus there is a lack of evidence-based optimal surgical management procedure. However, surgeons need to familiarize themselves with incarcerated appendixes within hernias in order to ensure potential successful surgical outcomes and avoid unexpected surgical complications. Thus, the aim of this paper is to provide new insight into the diagnosis and treatment of Amyand’s hernia and its complications.
Case Presentation
An 11-year-old boy presented with pain in the right groin region for 2 days. It was associated with mild fever, nausea and vomiting. Upon examination, a small lump in the right groin with inflammatory signs were noted. The records on investigations revealed that total WBC was 12, 60*10^9, C-reactive protein was 32 and an ultrasound image revealed that a small amount of free fluid was noticed in his right iliac fossa region, however, there wasn’t an appendix visualized. Clinically it was manifested as appendicitis. Thus, laparoscopically appendectomy was performed during the procedure findings were a ruptured appendix into the right side inguinal canal and the appendix was seen through the deep inguinal ring and entered into the inguinal canal. Also, the ruptured tip of the appendix and adherence to the cord structures were noticed. This patient had undergone appendectomy carefully without causing damage to the cord structures.
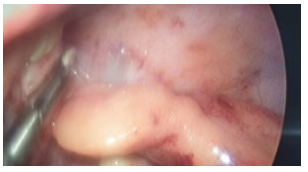
Figure 1: Inflammed appendix carefully delivered from the inguinal canal.

Figure 2: After delivery appendicectomy performed.
Discussion
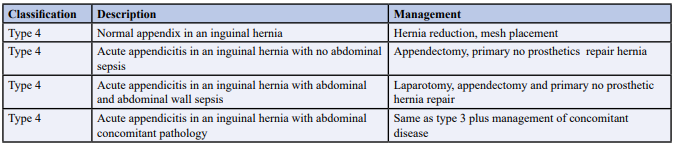
The most recurrent incidents of Amyand’s hernia accounted in men. Although the right side dominated significantly, also left side Amyand’s hernias were reported, it is due to situs inversus, intestinal malrotation, or a mobile cecum [4] it is quite challenging for clinicians to arrive at a pre-operative clinical diagnosis through physical examination although it can be achieved by the abdominal ultrasound or computed tomography [5]. The latter reveals that a tubular blind-ended structure originated from the cecum wall and extends to the hernia sac while the former indicates a similar finding of a blind-ended non-compressible tubular structure with increased vascularity. However, there is a lack of evidence-based diagnostic value of sensitivity and specificity to this particular clinical entity [6]. In our case, the patient had no clinical or biochemical data of compromised bowel thus any radiological images were not ordered. A classification system, which was proposed by Losanoff and Bassonin 2007 [7], clarifies the advocated surgical treatment selections for different types of Amyand’s hernias (Table 1). According to that, our patient was categorized as an Amyand type 1 hernia. Therefore no resection of the cecal appendix was performed and determined to be a micropore prosthetic polypropylene mesh. A study recommends reducing the hernia content but not performing tension hernia repair [8]. If an appendectomy is performed, a clean surgery needs to be combined with a clean-contaminated surgery due to raising the infection rate [9]. Although in the cases of inflamed, suppurative and perforated appendicitis no prosthetics material should be used as a result of the increased risk of surgical site infection and potential fistulae formation from the appendicular stump as well. In which cases an ice technique should be considered to ensure a lower recurrence rate in addition to appendectomy [10]. While it depends on various factors including the surgeon’s clinical decision, experience and domain over tension inguinal hernia repair techniques. However, existing new prosthetic materials like biological mesh influence the current surgical method in Amyand type 2 hernias as it suggests that the use of biological mesh prevents recurrence although there is a lack of literature to contend this hence future research needs to focus on its efficacy.
Table 1: A classification system and management of Amyand’s hernia [7].
Conclusion
In the clinical setting of an incarcerated complicated or strangulated inguinal hernia, the initial approach should consider imaging studies that could help to decide the surgical plan and enables the possibility of identifying involved intra-abdominal organs while management involves a laborious surgical technique and its definitive treatment will depend on the surgeon’s experience and clinical scenario.
Acknowledgement
The authors wish to thank, S.Thiruvarangan, Research Assistant who assisted in this manuscript preparation and submission process at the final stage.
References
1. Logan MT, Nottingham JM (2001) Amyand’s hernia: a case report of an incarcerated and perforated appendix within an inguinal hernia and review of the literature. Am Surg 67:628- 629.
2. Ali SM, Malik KA, Al-Qadhi H (2012) Amyand’s hernia: study of four cases and literature review. SQU Medical J 12:232-236.
3. House MG, Goldin SB, Chen H (2021) Perforated Amyand’s hernia. South Med J 94:496-498.
4. Al-Mayoof AF, Al-Ani BH (2013) Left-sided amyand hernia: report of two cases with review of literature. European J Pediatr Surg Rep 2(1):63-66.
5. Nicola SM (2007) Hernia de Amyand: presentacion de un caso y revisi on de la literatura. Rev ChilCirugía 59(2). 6. Mahajan A, Pawar P, Luther A, Haque P (2014) Right sided Amyand’s hernia: a rare case report. Int Surg J 1(1).
7. Losanoff JE, Basson MD (2007) Amyand hernia: what lies beneath-a proposed classification scheme to determine management. Am Surg 73(12):1288-1290.
8. Morales-Cárdenas A, Ploneda-Valencia CF, Sainz-Escárrega VH, Hernández-Campos AC, Navarro-Muñiz E, et al. (2015) Amyand hernia: Case report and review of the literature. Ann Med Surg (Lond) 4(2):113-115.
9. Hussain K, Aurangzeb, Ahmed M, Masood J (2014) Left sided Amyand’s hernia. J Coll Physicians Surg Pak 24(1):62.
10. Ramsingh Jason, Ali Ahmad, Cameron Caroline, Al-Ani Ahmed, Hodnett Robert, Chorushyj Catriona (2014) De Garengeot’s hernia: diagnosis and surgical management of a rare type of femoral hernia. J Surg Case Reports (2).