Case Report - (2024) Volume 2, Issue 6
Shingles on the Big Toe
2M.D. Republic of Turkey, Health Science University Izmir Bozyaka Research and Training Hospital, Fam, Turkey
Received Date: May 03, 2024 / Accepted Date: May 27, 2024 / Published Date: Jun 05, 2024
Copyright: ©©2024 Mehmet Sinan Saricicek, Ali Taylan Saricicek. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Saricicek, M. S., Saricicek, A. T. (2024).Shingles on the Big Toe. Int Internal Med J, 2(6), 01-03.
Abstract
Shingles occurs after reactivation of latent Varicella zoster virus (VZV) in the dorsal root ganglion. Usually, chickenpox is primary infection that occurs in childhood. After primary infection, VZV can be latent in neural tissue and can be reactive spontaneously or because of various risk factors. The most common risk factors are age >50 years, immunosuppression, infection, and mental stress. Symptoms appear in 3 phases: pre-eruptive, acute exudative, and chronic. Symptoms usually start in the pre-eruptive phase. Typically, patients present with painful or pruritic band-like vesicular lesions that do not cross the midline of the body. The most common site of shingles is the thoracic area. In this case report, we describe the atypical presentation of shingles with rare dermatomal involvement in a 55-year-old female patient who had a history of a significant immunocompromised state.
Keywords
Herpes Zoster, Hallux, Neuralgia, Pain
Introduction
Shingles occurs after reactivation of latent Varicella zoster virus (VZV) in the dorsal root ganglion [1–3]. Usually, the primary infection is chickenpox which is acquired in childhood. After primary infection, VZV can be latent in neural tissue and can be reactive spontaneously or because of various risk factors [2,3]. The most common risk factors are age >50 years, immunosuppression, infection and mental stress [1,2]. Symptoms appear in 3 phases: pre-eruptive, acute exudative and chronic [4]. Symptoms usually start in the pre-eruptive phase. Typically, patients present with painful or pruritic band-like vesicular lesions in the associated dermatome that do not cross the midline of the body [3].
Case:
Patient consented for both participating and publication of information
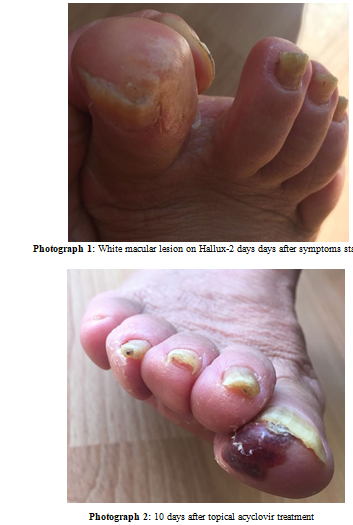
A 55-year-old female patient presented with pain in the left gluteal region that radiated to the left calf, ankle and left big toe. Her pain was described as burning and shocking. She reported that her symptoms started after lifting a heavy box. Her physical examination was normal. On the patient’s past medical history, there was ductal carcinoma of the breast and systemic sclerosis. The patient was treated with right mastectomy and axillary lymph node dissection followed by chemotherapy and radiotherapy. She was on letrozole, hydroxychloroquine, nifedipine and aspirin. She received her last chemotherapy 2 years ago. Her oncological and rheumatological routine controls were performed one week prior, and they were normal. A provisional diagnosis of musculoskeletal pain was made. Thiocolchicoside and paracetamol were prescribed. One day after her first presentation, she made a new appointment because of aggravated pain despite prescribed medications. On that occasion, she was suffering from burning pain in her left big toe. On physical examination, there were a few papular lesions that had not been present one day prior on her left gluteal region, calf and ankle. On her left big toe, there was a white macular lesion 2 mm in diameter (Photograph 1). She reported that she was using antifungal cream because of tinea pedis. A white macular lesion on the big toe was considered tinea pedis. Herpes zoster (HZ) was diagnosed for the other lesions compatible with the L5- S1 dermatomes. Topical acyclovir was initiated. On review visits, lesions on her gluteal region and calf gradually became specific herpetic lesions. The lesion on her left big toe widened, became papular in character and turned into a purplish, bullous lesion. A diagnosis of HZ was also made for lesion on the big toe. After a 10-day course of topical acyclovir treatment, papular and bullous lesions were abated with ecchymotic residue (Photograph 2). After 1 month, the ecchymosis on the big toe also abated without any scarring. Postherpetic neuralgia did not develop during follow-up.
Discussion
The definitive diagnosis of HZ is technically impossible before the lesions appear. Commonly, lesions of the HZ are observed on the thoracic area and do not cross the midline, but minding atypical involvement is very important. Pain can mimic musculoskeletal issues. If patient presents with pain, we need to add HZ to our differential diagnosis, especially in patients who have immunosuppression. The incidence of HZ and postherpetic neuralgia increase with age for which the initiation of treatment without any delay in elderly patients is very important for preventing complications such as postherpetic neuralgia.
Acknowledgment: This study was not funded by any organisation.
Author Contributions: All authors have contributed equally to the work. All authors read and approved the final manuscript.
Conflict of Interest: The authors declare that they have no potential conflict of interest in relation to the study in this paper.
This article was presented as a poster by Mehmet Sinan Saricicek in TAHUD 21. National Family Medicine Congress on 28/10/2022 12:30 under "Poster Presentations 1" session.
References
1. Atik, D., Taslidere, B., Bulut, B., DoÄ?an, S., Guven, R., and Cander, B. (2019). Can the Foot Pain Be the Varicella Zoster (Shingles)?. Eurasian Journal of Critical Care, 1(2), 81-84.
2. Beuerlein, K. G., and Strowd, L. C. (2019). Multidermatomal herpes zoster: a pain in the neck?. Dermatology Online Journal, 25(11).
3. Erdin, R., Soysal, B. A., and Dilcan, M. (2023). Zona zoster; an atypical presentation with severe pre-lesion pain: a case report. Journal of Medicine and Palliative Care, 4(6), 715- 717.
4. Patil, A., Goldust, M., and Wollina, U. (2022). Herpes zoster: a review of clinical manifestations and management. Viruses, 14(2), 192.