Research Article - (2024) Volume 9, Issue 2
Knowledge of the Pelvic Floor Muscles in Menopausal Women
Received Date: Jun 12, 2024 / Accepted Date: Jul 15, 2024 / Published Date: Jul 19, 2024
Copyright: ©©2024 Najwa Alfarra, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Alfarra, N., Aldosari, H., Aldwaish, A. (2024). Knowledge of the Pelvic Floor Muscles in Menopausal Women. Int J Womenâ??s Health Care, 9(2), 01-08.
Abstract
Introduction: Pelvic floor dysfunction is an important health-care issue, with menopause as the most important risk factors. Insufficient knowledge about pelvic floor dysfunction is the largest barrier to seeking care.
Aim of this Study: The aim of this study was to investigate the level of knowledge and information on pelvic floor dysfunction in menopausal women, and improve their awareness about the pelvic floor muscles.
Subjects and Methods: This study will use cross sectional survey. A valid and reliable questionnaire of 37 items was used as an online form. 100 women postmenopausal were included in the study. These were women aged 50 and above, who were able to read and use online form to participate in the study. Women who could not use on line survey were excluded from the study. All answers were analyzed and interpreted.
Results: The results of this survey showed minor actual knowledge about PFMs and PFD in PMP women, A major proportion of women would be interested in more information about PFMs. To improve help-seeking behavior in women but could also have a role in the prevention of PFD.
Conclusion: Knowledge of the PFM is necessary for the understanding of women over their own bodies, facilitating the understanding of guidelines and treatments offered by the health professionals.
Keywords
Pelvic Floor Muscles, Menopausal Pelvic Health, Pelvic Floor Exercises
Introduction
Pelvic floor dysfunction (PFD) is present in a wide range of clinical conditions, such as urinary incontinence, anal/fecal incontinence, pelvic organ prolapse, pelvic pain syndromes, sexual dysfunction, and defecation problems [1]. PFD occurs when the pelvic floor muscles are either weak or too tight or are incorrectly used. This issue is high prevalence, and impact quality of life. Therefore, PFD is considered an important health-care issue. Previous research suggested that insufficient knowledge and misperceptions about PFD are the largest barriers to seeking care [2]. Moreover, knowledge has been shown to improve compliance with pelvic floor muscle training and can induce behavioral changes [3]. In this study we will explore the knowledge of menopausal women about PFM and PFD, how can we improve menopausal women awareness about the PFM.
Methodology
• Design: Cross-sectional survey
• Sample: We planned to recruit at least 130 women. The study was carried out as an on-line survey. Due to the estimated dropout rate (the possibility of women misunderstanding the questions, leaving it blank, or overlooking it). We aimed to recruit at least 100 postmenopausal women
Inclusion Criteria
• Women over 50 years
• Menopausal status
• Able to read, write and use on line survey
• Mentally healthy
Exclusion Criteria
• Under 50 years
• Illiterate, or difficulty to use web site
Method
The patient recruited from the obstetrics /gynecology, urology, and physical therapy clinics. The researchers distributed soft copy of the survey to physicians, therapists, and ask them to pass it to the patient to fill it, if they are suitable to the study. The survey questionnaire adopted from Passmore et al., and Burns et al., [4,5]. The questionnaire consisted of 36 questions: three on demographic characteristics, 7 on gravidity and parity, 1 on menopause, 7 on pelvic floor structure and function, 8 on PFD and risk factors, 9 on education and gathering of information about this topic, and 1 on worries about pelvic floor Appendix 1
Questions were phrased in a socially and culturally sensitive manner, avoiding complex terminology. Succinct and unbiased response formats. Open and closed structured text, were used (depending on the information we intended to gather. Indecisive response options (e.g. I do not know and other) were included in order to enhance the response rates. Validity was examined by collecting expert opinions from three involved experts (1 Urologist, 1 pelvic floor therapist, and 1 gynecologist). The questionnaire was evaluated for face and content validity. A pilot study performed among the target population (15 volunteers) to evaluate whether respondents interpreted questions in a consistent manner, to judge the appropriateness of each included question, and to record the time required to complete the questionnaire.
Results
Assessment of content and face validity indicated that the questions were well interpreted and gave an accurate measurement of the concept and that the content assessed all fundamental aspects of PFMs and PFD. All women returned the questionnaire, giving a response rate of 100%. The time required to complete the questionnaire ranged from 7-15 minutes.
Demographic characteristics and gravidity–parity: 100 postmenopausal women (mean age 62.3; 50 to 67 years old) were included. The highest achieved degree of education was bachelor’s degree in 72 (72%), high school in 23 (23%), and primary school in 5 (5%). 58% housewife’s, and 41% working in different fields (physicians, teachers, lab technician, etc.…). PMP women had a mean gravidity of 2.8 (+/-1.6) and mean parity of 2.5 (+/-1.28). Last childbirth more than 20 years (65%), 34% (between 10-20 years), and 3% (less than 10 years). Vaginal birth 84% and C-section 16%. Higher number of episiotomies (65%). Non-instrumental vaginal deliveries were used. All PMP women declared that they were in the postmenopausal period.
Pelvic Floor Structure and Function
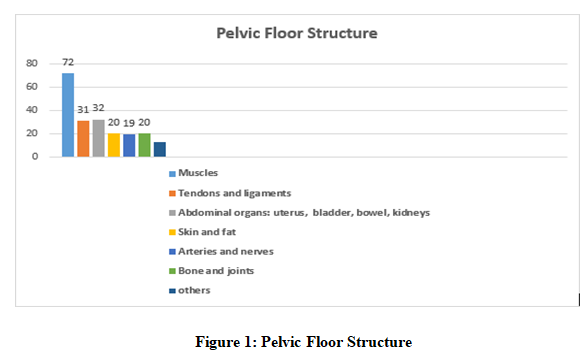
Most PMP women 72 knew that PF contains muscles. One-third of PMP women answered that the PF also includes bones, joints, internal organs, tendons, and ligaments. Furthermore, 19 of PMP women also thought the PF includes skin, fats, arteries and nerves in Figure 1
The majority of the participants located the PF correctly on the figure of the female body. On the other hand, 2% located the PF in the abdomen (above the ileum). 59% of the participants were aware that PFMs could be consciously contracted, and aware of the squeezing and lifting movement that the PFMs normally makes during an analytic contraction, whereas 41% of PMP women answered that they did not know what the PFMs do or why we need them. A greater portion of the women (86%) did not know how many normal anatomical openings there are in the female PF. Only (14%) answered three and were able to name them correctly.
The result for the questions about the occurrence of stress incontinence in the health people were answered 78% no, 22% do not know. 51% of the participants answered yes, 30% do not know, 18% no to the following question “is it normal that the pelvic floor muscles are not as strong after childbirth as before”. While 67% of the participants answered no, 33% yes to the question; “is it normal that a healthy woman experiences pain in the pelvic floor after childbirth”. 63% of them answered no, 26% do not know, 11% yes to the question “Is it normal that a healthy woman occasionally loses urine after childbirth”. While 9% of the participants answered yes, 59% no, and 32 do not know to this question; “is it normal that an average women experiences pain during intercourse after childbirth”. Greater percentage of the participants answered they do not know if the UI, and pain in the pelvic floor consequently expected after the vaginal delivery. 63% of the participants thought that the vaginal delivery causes more damage to the PFMs than fast vaginal delivery, vaginal delivery that takes longer, and cesarean. As well as 27% of the participants thought that a perineal rupture causes more damage to the PFMs than an episiotomy. Most of them answered that it is “the vagina” that tears during a perineal tear. Furthermore, the participants had no knowledge of POP.
Sexual Dysfunction
A greater percentage of PMP women answered did not know whether UI during sexual intercourse is normal, as well as they did not know what the PFMs doing through the intercourse, or if there is any relation with the orgasm.
Education and Gathering of Information
On a VAS scale 0-10 (0, no knowledge; 10 very high knowledge), the main ratings of the Postmenopausal (PMP) women for their general knowledge about the PF were 3/10 for 50 participants, 4 participants answered 6/10, while the rest of the participants answered from 1-2 out of 10. 74/100 participants never received information about the PF, while 26/74 women had received PFM information either during pregnancy, or pelvic floor rehabilitation sessions (Stress incontinence- prolapsed uterus). 27% of the participants received information about the pelvic floor muscles from the physiotherapist, 18% from the gynecology physicians, the rest from friends, books, and internet. 76/100 they never search for information about this topic on their own initiative. 80% of the participants did not have a good information about the pelvic floor muscles. While 71% were interested in more information on the topic.
Worries About PF
The majority does not have anxiety or fear about the PF (67%). While, 33% of the PMP women expressed a concern about urinary incontinence, or fear of prolapse.
Knowledge of PFD
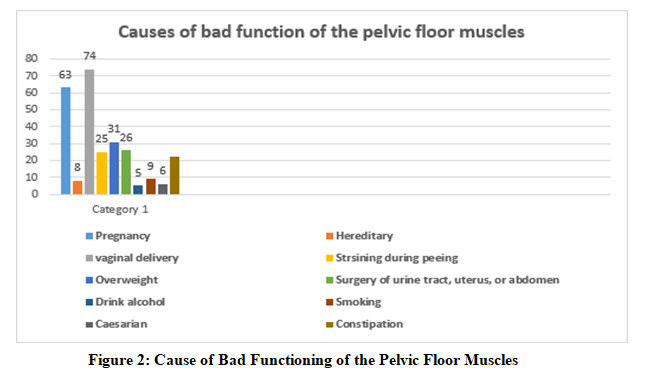
participants answered significantly more frequently that vaginal delivery 74%, multiple pregnancies 63%, obesity 31%, 26% surgery of urinary tract, uterus or abdomen, 25% straining during peeing, and 22% constipation (blockage of the bowels) can cause PFD, and the other causes were minor as shown in Figure 2.
Discussion
The results of this extended survey show minor actual knowledge about PFMs and PFD in PMP women. The questionnaire was not constructed to rate the degree of knowledge. The answers could not always be considered wright or wrong. On the contrary, the questions were constructed to reveal better comprehension of the current knowledge and ideas of women about this topic. All previous studies have focused on the knowledge of PFMT and not on the general knowledge women have about PFMs and PFD [6,7]. Mandimika et al., recently investigated the knowledge of UI and POP among community- dwelling women, with more pronounced knowledge gaps among nonwhite women. Our present study investigated the knowledge of a broad range of all PFD symptoms [2]. The results of the present study reveal slightly better actual knowledge with the participants who aged between 50-60 years old, and highly educated. Thus, we can conclude that the knowledge of younger and bachelor degree women about the PFMs and PFD differ with age and level of education. Participants showed the same trend in acceptance of PFD symptoms after delivery: most women agree that certain PFD symptoms could be considered normal immediately after childbirth but should improve or disappear after 3 to 6 months. In our opinion , it is important to use education about this topic to prevent women from accepting PFD symptoms and to empower help-seeking behavior.
It is remarkable that more than 70% of the participants ever received information about the PF and that a majority them would welcome more information. When information was provided, it was mostly during pregnancy or during PF rehabilitation sessions, which is late. The participants were significantly better aware of PFD risk factors such as multiple vaginal deliveries, multiple pregnancies, obesity, and constipation. Better knowledge of these symptoms and contributing factors, could affect help-seeking behavior and positively influence prevention of PFD [2]. Information about the PF was received rather late in life, so timely prevention was not possible. This shows that there is work to be done to better inform all women. One can only encourage the trend that we observed that more women these days are already getting informed about this topic during their childbearing years. Nevertheless, the results of this study confirmed the need to reach more women with good information, and the authors suggested information should be offered repeatedly by ensure it is not forgotten. Improved knowledge about such things as bladder behavior, PFM exercises, and stool habits would likely make a great difference. Further work in needed to determine how such education should be provided and who should provide it.
In 2013, Buurman et al, performed a qualitative research about women’s perceptions about PFD and their help-seeking behavior [8]. Several women explicitly mentioned embarrassment as an impediment for seeking help. In general, PF problems are still a taboo for most women. The low number of women in our study that took active steps to get help or information confirms these statements. Our results clearly reveal that the majority of women of all ages are aware of the problem, feel badly informed, and are interested in more information. This is a strong argument further work on improving and intensifying PF education. Future research must investigate how women would like to be informed and which campaigns would be the most effective, with the best compliance. To conclude there is sparse knowledge about the pelvic floor among women. Most postmenopausal women get informed during the postmenopausal period, which is very late. A major proportion of women would be interested in more information. Improving common knowledge about PFMs and PFD could improve help- seeking behavior in women but could also have a role in the prevention of PFD.
The Limitation of the Study
No published study in that field previously. The online design of this study limited the number of participants as it could not include those who were unable to use smartphones and computers. However, organizing the study online allowed women from different cities and regions of the country to participate.
Conclusion
Knowledge of the PFM is necessary for the understanding of women over their own bodies, facilitating the understanding of guidelines and treatments offered by the health professionals [9].
References
1. Bortolini, M. A. T., Drutz, H. P., Lovatsis, D., & Alarab, M. (2010). Vaginal delivery and pelvic floor dysfunction: current evidence and implications for future research. International urogynecology journal, 21, 1025-1030.
2. Mandimika, C. L., Murk, W., McPencow, A. M., Lake, A., Wedderburn, T., Collier, C. H., ... & Guess, M. K. (2014). Knowledge of pelvic floor disorders in a population of community-dwelling women. American journal of obstetrics and gynecology, 210(2), 165-e1.
3. Shah, A. D., Shott, S., Kohli, N., Wu, J. M., Catlin, S., & Hoyte, L. (2008). Do racial differences in knowledge about urogynecologic issues exist?. International Urogynecology Journal, 19, 1371-1378.
4. Passmore, C., Dobbie, A. E., Parchman, M., & Tysinger, J. (2002). Guidelines for constructing a survey. FAMILY MEDICINE-KANSAS CITY-, 34(4), 281-286.
5. Burns, K. E., Duffett, M., Kho, M. E., Meade, M. O., Adhikari, N. K., Sinuff, T., & Cook, D. J. (2008). A guide for the design and conduct of self-administered surveys of clinicians. Cmaj, 179(3), 245-252.
6. Whitford, H. M., Alder, B., & Jones, M. (2007). A cross- sectional study of knowledge and practice of pelvic floor exercises during pregnancy and associated symptoms of stress urinary incontinence in North-East Scotland. Midwifery, 23(2), 204-217.
7. Liao, Y. M., Dougherty, M. C., Liou, Y. S., & Tseng, J. (2006). Pelvic floor muscle training effect on urinary incontinence knowledge, attitudes, and severity: an experimental study. International journal of nursing studies, 43(1), 29-37.
8. Buurman, M. B. R., & Lagroâ?Janssen, A. L. M. (2013). Women’s perception of postpartum pelvic floor dysfunction and their helpâ?seeking behaviour: a qualitative interview study. Scandinavian journal of caring sciences, 27(2), 406- 413.
9. Buckley, B. S., & Lapitan, M. C. (2010). Epidemiology Committee of the Fourth International Consultation on Incontinence, Paris, 2008. Prevalence of urinary incontinence in men, women, and children--current evidence: findings of the Fourth International Consultation on Incontinence. Urology, 76(2), 265-70.
Appendix
Appendix 1: Questionnaire
Dear Madam,
The purpose of this study is to improve the prevention and the treatment of pelvic floor disorders. Through the questionnaire below, we try to explore the current knowledge of women about the pelvis and pelvic floor muscles. Therefore, we would like you to respond spontaneously to these questions without searching for the correct answers in books or on the internet. This survey is completely anonymous, completion takes about 20 minutes of your time. Thank you for your cooperation. Occasionally we will ask you some open answer questions. Please fill in the thoughts that first come into your mind.
1. How old are you?
• 50-60 years
• More than 60 years
2. Mark your highest degree of education:
• Elementary school
• High school
• University
3. What is your current occupation?
• House wife
• Others
4. How many times have you been pregnant?
• 1-3 times
• 3-6 times
• More than 7 times
5. In which year did you last give birth?
• Less than 10 years
• 10-20 years
• More than 20 years
6. Type of delivery:
• Vaginal: Yes No
• Did they have to cut? Yes No
• Cesarean Yes No
• Forceps Yes No
• Vacuum extraction Yes No
7. Are you postmenopausal?
Yes No
8. What is included in the pelvic floor? Multiple answers
are possible.
• Muscles
• Tendons and ligament
• Abdominal organs: uterus, bladder, bowel, kidneys
• Skin and fat
• Arteries and nerves
• Bone and joints
• Others
9. Where can you localize the pelvic floor muscles?
Please mark on the graph.
10. What do the pelvic floor muscles do?
• I do not know
• Others
11. Why do we need them?
• I do not know
• Others
12. Is a healthy woman able to control (contract and relax) the pelvic floor muscles whenever she wants?
• Yes
• No
• I do not know
13. Which movement do the pelvic floor muscles make? Please mark, multiple answers are possible.
• Pinching movement
• Inwards lifting movement
• Outward pushing movement
• No conscious control possible.
• I don’t know
14. How many openings do women have in the pelvic floor?
15. Which is the possible cause of bad functioning of the pelvic floor muscles? Please mark the three most common causes.
• Pregnancy
• Heredity
• Vaginal delivery
• Straining during peeing
• Overweight (obesity)
• Surgery of urinary tract, uterus or abdomen
• Drinking alcohol
• Smoking
• Caesarean
• Constipation (blockage of the bowels)
16. Does a healthy person occasionally lose urine?
Yes No
17. Does a healthy person lose urine during exercise or effort, such as intensive sports?
Yes No I don’t know
18. Do you find it normal if women daily use a precautionary pad to control urine leakage?
Yes No I don’t know
19. Are the pelvic floor muscles not as before, after childbirth?
Yes No I don’t know
If yes, mark which consequences after childbirth are normal, multiple answers are possible:
• Gapping vagina
• Involuntary loss of urine
• Stool problems (blockage , diarrhea)
• Flatulence.
• Pain in the pelvic floor
• Pain during intercourse
• Diminished orgasm during intercourse.
20. Does a healthy woman experiences pain in the pelvic floor?
• Immediately after delivery Yes No I don’t know
• 1 month after delivery Yes No I don’t know
• 6 months after delivery Yes No I don’t know
21. Does a healthy woman occasionally lose urine?
• Immediately after delivery Yes No I don’t know
• 1 month after delivery Yes No I don’t know
• 6 months after delivery Yes No I don’t know
22. Does a healthy woman occasionally loses stool?
• Immediately after delivery Yes No I don’t know
• 1 month after delivery Yes No I don’t know
• 6 months after delivery Yes No I don’t know
23. Does an average women experiences pain during intercourse?
• Immediately after delivery Yes No I don’t know
• 1 month after delivery Yes No I don’t know
• 6 months after delivery Yes No I don’t know
24. Circle per each line which way of delivery may have the most negative consequences for the pelvic floor muscles:
• Caesarean Section OR vaginal delivery
• Fast vaginal delivery OR vaginal delivery that takes longer
• Vaginal delivery with episiotomy (cuts) OR vaginal delivery with rupture (tear)
• Vaginal delivery with spoons /forceps OR vaginal delivery with vacuum
25. What can be cut or tear during vaginal delivery?
• I don’t know
26. What does the term “prolapse/sagging in the small basin” means for you?
• I don’t know
27. Do pelvic floor muscles play a role in getting a sexual orgasm?
• Yes No I don’t know
28. Does a healthy woman frequently experience pain during sexual intercourse?
• Yes No I don’t know
29. Does a healthy woman leak a little bit urine during sexual intercourse?
• Yes No I don’t know
30. Do you know the therapy that is given to woman with pelvic floor problems?
• Yes No I don’t know
31. Did you ever receive pelvic floor therapy?
• Yes No
If yes, why
32. How much do you know about the pelvic floor muscles on a scale from zero to ten, whereas, zero is absolutely nothing and ten is expert in the domain?
33. Did you ever receive information about the pelvic floor muscles?
• Yes No
If yes: When
For which reason
From who/what? Multiple answers to select
• Gynecologist
• Friends /family
• Physiotherapist
• Nurse
• Midwife
• School
• General practitioner
• Others
34. Did you ever search for information about this topic on your own initiative?
• Yes No
If yes: select answers:
• Books
• Physiotherapist
• Internet
• Friends/family
• Gynecologist
• General practitioner
• Others
35. Do you find yourself good informed about the pelvic floor muscles?
• Yes No
36. Do you want more information about the pelvic floor muscles?
• Yes No
37. Which is your biggest anxiety or fear about the pelvic floor?
• I don’t know
• None
Thank you for filling this survey


