Research Article - (2025) Volume 4, Issue 1
Incidence and Outcome of Readmission of Surgical Patients to Intensive Care Unit and Associated Factors at Tikur Anbessa Specialized Hospital Prospective Observational Study
Received Date: Jan 09, 2025 / Accepted Date: Mar 17, 2025 / Published Date: Mar 25, 2025
Copyright: ©©2025 Osman Aman Hamido, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Hamido, O. A., Denberu, Y. D., Shafi, A. S., Bulto, Y. B., Tafesse, B. A. (2025). Incidence and Outcome of Readmission of Surgical Patients to Intensive Care Unit and Associated Factors at Tikur Anbessa Specialized Hospital Prospective Observational Study. J Surg Care. 4(1), 01-08.
Abstract
Background Globally, advancements in critical care have significantly improved survival rates for critically ill patients. However, the availability and high cost of intensive care facilities remain major challenges, especially in developing countries. ICU readmission, defined as a patient’s deterioration during the same hospitalization necessitating a return to the ICU, is associated with poor outcomes and increased costs. While most studies on ICU readmissions are conducted in developed nations, little is known about its epidemiology, causes, and outcomes in Ethiopia.
Objective To determine the incidence, associated factors, and outcomes of surgical ICU readmissions at Tikur Anbessa Specialized Hospital (TASH) from September 2023 to February 2024.
Methodology This prospective, institution-based study was conducted from September 1, 2023, to February 29, 2024. Data were collected using prepared checklists from patient charts and analyzed with SPSS version 27. Descriptive statistics were used for continuous variables, and bivariate logistic regression was performed for predictor and outcome variables. Multiple logistic regression identified significant factors, with p-values <0.05 considered statistically significant.
Results Among 186 patients transferred from the ICU to the ward, 12 (6.5%) required readmission. Oxygen requirement during transfer significantly increased the likelihood of readmission (AOR 5.6, 95% CI: 1.367–23.439). Of the readmitted patients, 41.7% recovered, while 58.3% died.
Conclusion Oxygen requirement during transfer to the ward was a major risk factor for ICU readmission. Readmitted patients had poor outcomes, with a mortality rate of 58.3%.
Keywords
Surgical Intensive, Care, Unit, Readmission, Outcome
Introduction
Globally, advancements in critical care treatment have significantly improved the survival rates of critically ill patients. However, the scarcity and high cost of intensive care facilities remain pressing challenges, particularly in developing countries. These issues are compounded by the additional strain placed on patients and healthcare systems due to unanticipated readmissions to the intensive care unit [1,2]. Hospitals employ quality metrics to evaluate various aspects of patient care, with ICU readmission being one critical metric. ICU readmission refers to the re-admittance of a patient to the intensive care unit during the same hospital stay after a prior discharge. Advances in critical care medicine have significantly improved the survival rates of critically ill patients worldwide. However, in developing countries, the scarcity of intensive care facilities and financial constraints often necessitate the early discharge of patients from ICUs, posing challenges to their recovery and outcomes [3–6].
Timely discharge from the ICU helps minimize excessive and unnecessary utilization of this costly healthcare resource while ensuring bed availability for other critically ill patients. However, this practice often transitions patients to lower levels of care on general wards, which may lack the resources to adequately address their needs. Such transitions can increase the risk of clinical deterioration and even mortality. In this context, optimizing available resources and prioritizing healthcare quality management are critical to maintaining an effective and sustainable health system [7–9]. Intensive care medicine has advanced considerably, now accounting for a significant portion of healthcare expenditures in many countries. This financial burden is especially pronounced in low-income nations. The transition of patients from the ICU to hospital wards represents a critical and vulnerable phase in healthcare delivery. This vulnerability arises from several factors, including the transfer of critically ill patients from a resource-rich ICU environment to wards with fewer resources, the involvement of multiple providers, the absence of standardized discharge protocols, and communication challenges—both verbal and written—among providers and between providers and patients [10–12].
ICU readmission occurs when a patient’s condition deteriorates during the same hospital stay, necessitating a return to the ICU for further treatment. Such readmissions are often associated with poor prognoses, and the resulting increase in hospitalization costs places a significant financial burden on both patients’ families and the healthcare system [2,13]. Although a multicenter retrospective study conducted in Addis Ababa identified an association between ICU readmissions and mortality, there is a lack of research on the specific causes and risk factors of ICU readmissions. Understanding these factors would empower ICU teams to optimize discharge planning and improve ongoing care for patients transitioning out of the ICU [14–17]. This study aims to determine the incidence, risk factors, and outcomes of patients readmitted to the surgical intensive care unit at Tikur Anbessa Specialized Hospital. While studies conducted primarily in developed countries have established a link between ICU readmissions and adverse outcomes, there is a significant gap in research within our context. Understanding the incidence, causes, and outcomes of ICU readmissions is essential to gauge the magnitude of the problem, identify associated factors, and determine predictors of poor outcomes. Additionally, this study can serve as a foundation for future research in this area.
Objectives
To assess the magnitude, associated factors and outcomes of readmission to surgical ICU at TASH from September 2023 to February 2024
Method
The study was conducted from September 1, 2023 to February 29, 2024 at Tikur Anbessa Specialized Hospital in Addis Ababa, Ethiopia. TASH is the largest referral and teaching governmental hospital in Ethiopia with 700 beds, accommodating referred patients from all over the country and has most specialties and subspecialties. The hospital has one main ICU and one cardiac ICU. The main ICU has 16 beds of which 6 beds are dedicated for Surgical ICU and run by Anesthesiologist, 6 beds for Medical ICU run by pulmonologist and 4 beds for Pediatrics run by pediatric pulmonologist.
Study Design
Institutional Based Prospective, Observational Study
• Population: Source Population All adult patients admitted to TASH Surgical ICU and discharged alive during the study period
• Study Population All adult patients who are readmitted to Surgical ICU within the study period and met the inclusion criteria.
Eligibility Criteria
• Inclusion Criteria
All adult patients admitted to SICU and discharged alive from SICU.
• Exclusion Criteria
Scheduled readmission due to elective surgical procedure, Age < 18yrs, Patient directly discharged to home or referred to other hospital, and Patient that went against medical advice
Sample Size Determination and Procedure
• Sample Size Determination All patients who are admitted to SICU in the study period will be included in the study.
• Sampling Procedure Institutional based census sampling will be used
Variables of the Study
• Dependent Variable ICU readmission, ICU Outcome
• Independent Variables Sociodemographic Age, Sex, BMI, Clinical Characteristic during initial admission, Admission diagnosis/reason, Type of surgery, Respiratory status, GCS, Mechanical ventilator use, Inotrope requirement, Oxygen requirement, Comorbidities, Patient condition during transfer, On tracheostomy, Oxygen requirement, Transfer time
Operational Definition
• ICU Readmission admission to intensive care unit of a patient previously admitted to the ICU during the same hospital encounter
• Co-Morbidity Diseases or disorders that exist together with an index disease or co-occurrence of two or more diseases or disorders in an individual.
• Outcome surgical ICU outcome
Data Collection Procedure
The data was collected using a structured questionnaire from patient chart by year 2 and year 3 anesthesiology residents who were trained for collecting this data. Data was collected from eligible patients using structured questionnaires with simultaneous crosschecking of data from patients’ chart for consistency and reliability of clinical characteristics. The patients’ unique identification number through medical record was strictly applied to avoid repetitions. The data was collected from September 1, 2023 to February 29, 2024. The questionnaires were checked for completeness, consistency, clarity and accuracy at the end of data collection day.
Data Processing and Analysis
Data was checked for completeness and then imported to SPSS version 27 software for analysis. Descriptive statistics was used to describe the study variables. Association of each independent variable and dependent variable was assessed by bivariate followed by multivariate logistic regression analysis after testing for fitness of the model using Hosmer and Lemisho goodness of fit model for this analysis. Multicollinearity was checked among independent variables and the effect of confounders was controlled during the analysis process using multivariable analysis. Those independent variables with P-value < 0.25 in the bivariate analysis was taken into multivariable logistic regression analysis. Adjusted odds ratio with 95% CI was employed to control confounding effect. P value of < 0.05 was used to declare statistical significance for association of the dependent and the independent variables.
Ethical Consideration
Prior to data collection ethical clearance was obtained from ethical review committee of Addis Ababa University, College of health sciences. Verbal informed consent was obtained from the patient before data was collected. Information obtained from this data will only be used for the purpose of this research and confidentiality will be kept for all patients.
Dissemination Plan
The result of the study was submitted to AAU school of medicine, department of Anesthesiology and critical care, ICU directorate and other Hospital administrative staff. Results, and Library of College of Health Sciences
Results
Sociodemographic Data
In this study 186 patients were transferred from SICU to the wards during the 6 months study period. 96(51.6 %) of them were males and 90(48.4%) accounts for female. Their age ranged from 18 to 82 with a mean age of 41.6 yrs. Majority of patients 170(91.4%) had normal BMI, 10(5.4%) were underweight, 5(2.7%) were overweight and 1(0.5%) patient were obese.
|
Variables |
Frequency |
Percent |
|
|
Sex |
Male |
96 |
51.6 |
|
Female |
90 |
48.4 |
|
|
Age(yrs) |
18-34 |
66 |
35.5 |
|
35-49 |
60 |
32.3 |
|
|
50-69 |
51 |
27.4 |
|
|
>=70 |
9 |
4.8 |
|
|
Mean age |
41.6 |
||
|
BMI |
<18.5 |
10 |
5.4 |
|
18.5-24.9 |
170 |
91.4 |
|
|
25-29.9 |
5 |
2.7 |
|
|
30-34.9 |
1 |
0.5 |
|
Table 1: Frequency Distribution of Sociodemographic Characteristic of Patients Transferred from SICU at TASH SICU from September 2023 – February 2024
Clinical Characteristic of Patient During Initial ICU Admission
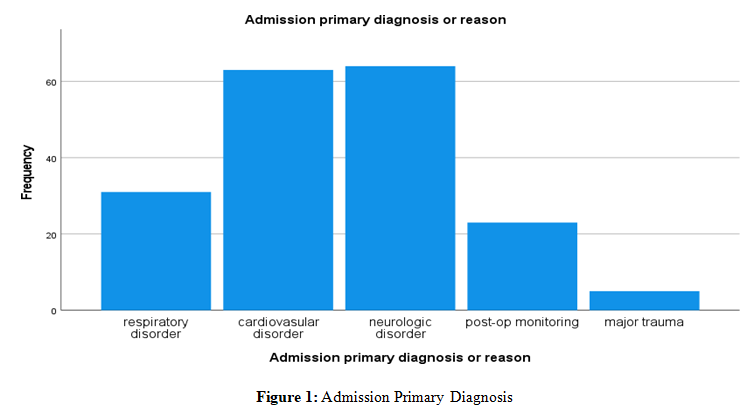
In the primary admission to SICU, majority 175(94.1%) were from operating room, 5(2.7%) were direct admissions from the emergency, 5(2.7%) from ward and the rest 1(0.5%) patient were from other hospital. Of the total 186 patients, 133(71.5%) had an elective surgery, 47(25.3%) had an emergency surgery and 6(3.2%) had not undergone any surgical procedure. Majority 78(43.3%) of the patients had neurosurgical procedure, followed by Thoracic surgery 27(15%), Genera surgery 22(12.2%), Obstetric and Gynecologic surgery 19(10.6%), Vascular surgery 13(7.2%) and orthopedic surgery 9(5%). Most of the patients (61.3%) had good respiratory status while 38.6% were in distress.
|
Variables |
|
Frequency |
Percent |
|
Source of admission |
Emergency room |
5 |
2.7 |
|
Operating room |
175 |
94.1 |
|
|
Ward |
5 |
2.7 |
|
|
Other hospital |
1 |
0.5 |
|
|
Type of surgery |
Emergency |
47 |
25.3 |
|
Elective |
133 |
71.5 |
|
|
Type of procedure |
General surgery |
22 |
12.2 |
|
Neurologic Surgery |
78 |
43.3 |
|
|
Thoracic Surgery |
27 |
15 |
|
|
Obstetric and gynecologic |
19 |
10.6 |
|
|
Orthopedic Surgery |
9 |
5 |
|
|
Vascular Surgery |
13 |
7.2 |
|
|
ENT Surgery |
8 |
4.4 |
|
|
Urologic surgery |
4 |
2.2 |
|
|
Respiratory status |
Normal |
114 |
61.3 |
|
In distress |
72 |
38.6 |
|
|
GCS |
15 |
134 |
72 |
|
13-14 |
8 |
4.2 |
|
|
9-12 |
11 |
5.9 |
|
|
<9 |
9 |
4.8 |
|
|
Sedated |
24 |
12.9 |
|
|
Need of MV support |
Yes |
49 |
26.3 |
|
No |
137 |
73.6 |
|
|
Inotrope requirement |
Yes |
19 |
10.2 |
|
No |
167 |
89.7 |
Table 2: Characteristic of Patients During Initial ICU Admission at TASH
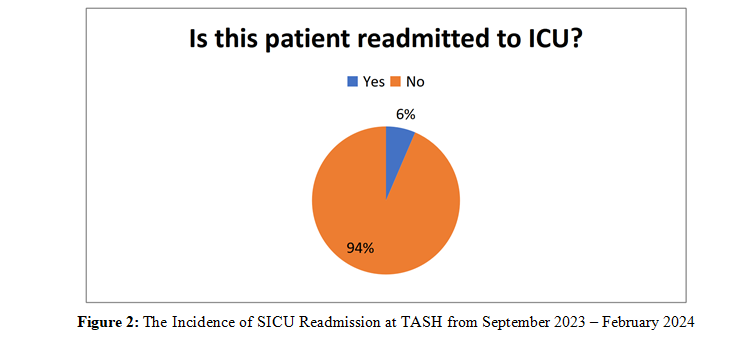
Incidence of SICU Readmission
Among 186 patients that were transferred during the study period, 12(6.5%) were readmitted.
Factors Associated with Readmission
To identify factors associated with readmission, first simple logistic regression was performed to select candidate variables that had crude association with static utilization at P-value <0.25% Initially all independent variables were entered in the bi- variate logistic regression model in order to determine the factors associated with readmission. On the bi-variate logistic regression model, those variables with a p-value less than 0.25 were selected as a candidate variable. Then the selected variables were subjected to multiple logistic regression. Finally, a step-down method of multivariate logistic regression was carried out for the variable’s respiratory status during initial ICU admission, Glasgow coma scale, need of mechanical ventilation support and oxygen support requirement during transfer to ward. A P value less than 0.05 was considered statistically significant and presented with 95% CI and AOR. Accordingly, only oxygen requirement during transfer from ICU to ward were found to have significant association s with ICU readmission. In this study patients who required oxygen support during transfer from ICU to ward were five times more likely to be readmitted to ICU as compared to those who didn’t require oxygen support (AOR =5.6, CI 1.367 -23.439, (P=0.017)).
|
VARIABLE |
READMISSION TO SICU |
NON-READMISSION TO SICU |
|||
|
Number |
Percent |
Number |
Percent |
||
|
Sex |
Male |
6 |
3.25 |
89 |
47.8 |
|
Female |
6 |
3.25 |
85 |
45.7 |
|
|
Source of admission |
Emergency room |
1 |
0.5 |
4 |
|
|
Operating room |
10 |
5.3 |
165 |
88.7 |
|
|
Ward |
1 |
0.5 |
4 |
2.1 |
|
|
Other hospital |
|
|
1 |
0.5 |
|
|
Admission primary diagnosis |
Respiratory disorder |
2 |
1.1 |
28 |
15 |
|
Cardiovascular disorder |
3 |
1.6 |
59 |
31.7 |
|
|
Neurologic disorder |
5 |
2.7 |
61 |
32.8 |
|
|
Trauma |
2 |
1.1 |
3 |
1.6 |
|
|
Post opp. monitoring |
|
|
23 |
12.3 |
|
|
Oxygen requirement during transfer |
Yes |
7 |
3.7 |
12 |
6.4 |
|
No |
5 |
2.7 |
162 |
87.1 |
|
|
Time of Transfer to ward |
Day time |
11 |
5.9 |
170 |
91.4 |
|
Evening |
|
|
1 |
0.5 |
|
|
Weekend |
1 |
0.5 |
3 |
1.6 |
|
|
Inotrope requirement |
Yes |
2 |
1.1 |
17 |
9.1 |
|
No |
10 |
5.3 |
157 |
84.4 |
|
|
Glasgow coma scale |
15 |
5 |
2.6 |
129 |
69.4 |
|
13-14 |
1 |
0.5 |
7 |
3.7 |
|
|
9-12 |
|
|
11 |
5.9 |
|
|
<9 |
2 |
1.1 |
7 |
3.7 |
|
|
Sedated |
4 |
2.1 |
20 |
10.8 |
|
|
Need mechanical ventilation |
Yes |
9 |
4.8 |
40 |
21.5 |
|
No |
3 |
1.6 |
134 |
72 |
|
|
Respiratory Status |
Normal |
2 |
1.1 |
112 |
60.2 |
|
In distress |
10 |
5.3 |
62 |
33.3 |
|
Table 3: Frequency of Different Variables for Readmitted and Non-Readmitted Patients at TASH, 2024
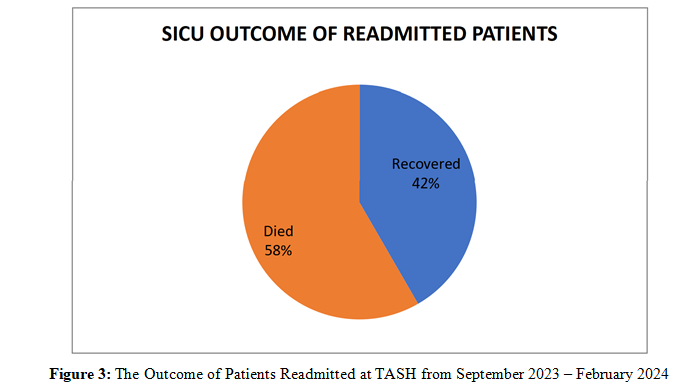
SICU Outcome of Readmitted Patients
Among 12 patients that were readmitted during the study period, 5(41.7%) patients recovered and 7(58.3%) died.
|
VARIABLE |
Sig. |
AOR |
95% C.I for EXP(B) |
||
|
Lower |
Upper |
||||
|
|
Respiratory status in distress |
.062 |
4.807 |
0.926 |
25.282 |
|
|
Need of mechanical ventilation |
.071 |
6.403 |
0.0840 |
49.498 |
|
|
Does the patient require oxygen support during transfer to ward? |
.017 |
5.612 |
1.367 |
23.432 |
Table 4: Multivariate Analysis to Identify Factors Associated with ICU Readmission at TASH, 2024
Discussion
In this prospective study, from 186 surgically admitted ICU patients, 12 of patients required readmission during the same hospitalization having the readmission rate of 6.5%. The study done in Brazil reported readmission rate was 10% (n= 576/5,779) [2]. Similarly, Mohammed et al, reported readmission rate of 10.3%(n=25/242) [18]. This could be due to the difference of ICU admitted patient in this study which are mainly planned neurological and thoracic surgery patients which are relatively younger (41.6 Vs 61.6) and has less comorbidities. In addition, these studies were done in medico-surgical ICU patients and over longer duration compared with this 6-month study. This finding is reported SICU readmission rate of 13.4% [19]. However, it is comparable with Rosenberg and Watts systemic review report of 7% readmission rate [20]. Though it is one of ICU quality metrics there is no local data available regarding the frequency of ICU readmission in our set up. So, this is probably the first study regarding the SICU readmission conducted in Ethiopia.
In contrast to previous studies that reported multiple factors like; evening time discharge, comorbidity, neurological disorders, cardiovascular disorders, use of vasopressors, mechanical ventilation, presence of malignancy as major risk factor for readmission, this study found only oxygen requirement during transfer to ward as main risk factor for ICU readmission. We observed no statistically significant association between readmission rates and factors such as respiratory distress, low GCS, evening time discharge, comorbidity, neurological disorders, cardiovascular disorders, use of vasopressors, mechanical ventilation, despite numerical percentage differences. Although the need of mechanical ventilator, need of inotrope use, trauma patients, those with GCS< 9 and patients in respiratory distress showed no statistical significance in our study, they had notably higher readmission probabilities. Only 5/12(41.7%) of readmitted patients were recovered and the rest 7/12(58.3.%) patients were died in this study. A multicenter retrospective study done in Addis Ababa on survival status and predictors of mortality among patients admitted to SICU identified that readmission to SICU is one of the predictors of mortality in SICU [14]. This is in agreement with the high mortality (58.3%) of readmitted patient in this study. Finally, our results may not apply to other ICUs with a different case mix such as medical or mixed medico-surgical ICU patients.
Strength and Limitations of the Study
This study has some limitations. First, due to the observational nature of the study we could not determine whether readmissions were appropriate or not. Second the relatively short study period and the absence of studies done in Ethiopia affect strong discussion. Furthermore, the lack blood gas tests and other lab results that may have influenced the result can be mentioned as limitation.
Conclusion
In conclusion, the incidence of surgical ICU readmission in this study is 6.5%. The oxygen requirement during transfer to ward was strongly associated with readmission. The readmission to ICU was also found to result in poor outcome with 58.3% mortality among readmitted patient. This data provides important insights into the incidence, risk factors for readmission and SICU outcome of readmitted patients.
Recommendations
In accordance to the findings in this study, we propose the following recommendations.
• Risk stratification of patients discharged from ICU.
• Step down unit should be prepared for high-risk patients transferred from ICU.
• Further study shall be conducted in our set-up
Declarations
Declaration of Figures authenticity.There is no picture taken for this manuscript
Authors Contribution
OA prepared the manuscript and conceptualized and edited it by
YD. All others reviewed the manuscript.
Ethical Approval and consent to participate
Ethical Clearance was obtained from Department of Anesthesiology
Ethical Clearance board, Tikur Anbessa Specialized Hospital,
Addis Ababa University (DOS/RES/REC/50/2023) and we obtained informed oral consent from each patient to collect the questioner
Consent for Publication
Written informed consent was obtained from Ethical Clearance board. Written consent is available (DOS/RES/REC/50/2023) for review.
Availability of Data
Data were analyzed/generated using SPSS version 26 during this thesis
Competing Interest
none
Funding
None
Authors Contribution
OA prepared the manuscript and conceptualized and edited it by
YD. All others reviewed the manuscript.
Acknowledgements
We would like to thank the department of Anesthesiology, critical care and pain medicine for this opportunity to do this thesis. We also want to forward our gratitude advisors Dr. Yonathan and Dr. Amria for constructive input and advice, and Dr. Betenas Ayalew and Dr. Yidersal Demsie in analysis of data and editing for this manuscript. Lastly, we would like to express our gratitude for colleagues, families and friends for unwavering support during preparation of this research
References
1. Murthy, S., Leligdowicz, A., & Adhikari, N. K. (2015). Intensive care unit capacity in low-income countries: a systematic review. PloS one, 10(1), e0116949.
2. Ponzoni, C. R., Corrêa, T. D., Filho, R. R., Serpa Neto, A., Assunção, M. S., Pardini, A., & Schettino, G. P. (2017). Readmission to the intensive care unit: incidence, risk factors, resource use, and outcomes. A retrospective cohort study. Annals of the American Thoracic Society, 14(8), 1312- 1319.
3. Losonczy, L. I., Papali, A., Kivlehan, S., Hynes, E. J. C., Calderon, G., Laytin, A., ... & Reynolds, T. (2021). White paper on early critical care services in low resource settings. Annals of global health, 87(1).
4. Brown, S. E., Ratcliffe, S. J., & Halpern, S. D. (2015). Assessing the utility of ICU readmissions as a quality metric: an analysis of changes mediated by residency work-hour reforms. Chest, 147(3), 626-636.
5. Ponzoni, C. R., Corrêa, T. D., Filho, R. R., Serpa Neto, A., Assunção, M. S., Pardini, A., & Schettino, G. P. (2017). Readmission to the intensive care unit: incidence, risk factors, resource use, and outcomes. A retrospective cohort study. Annals of the American Thoracic Society, 14(8), 1312- 1319.
6. Mcneill, H., & Khairat, S. (2020). Impact of intensive care unit readmissions on patient outcomes and the evaluation of the national early warning score to prevent readmissions: literature review. JMIR perioperative medicine, 3(1), e13782.
7. Hosein, F. S., Roberts, D. J., Turin, T. C., Zygun, D., Ghali,
W. A., & Stelfox, H. T. (2014). A meta-analysis to derive literature-based benchmarks for readmission and hospital mortality after patient discharge from intensive care. Critical Care, 18, 1-12.
8. Stelfox, H. T., Soo, A., Niven, D. J., Fiest, K. M., Wunsch, H., Rowan, K. M., & Bagshaw, S. M. (2018). Assessment of the safety of discharging select patients directly home from the intensive care unit: a multicenter population-based cohort study. JAMA internal medicine, 178(10), 1390-1399.
9. Chan, C. W., Farias, V. F., Bambos, N., & Escobar, G. J. (2012). Optimizing intensive care unit discharge decisions with patient readmissions. Operations research, 60(6), 1323- 1341.
10. Turner, H. C., Van Hao, N., Yacoub, S., Clifton, D. A., Thwaites, G. E., Dondorp, A. M., ... & Chau, N. V. V. (2019). Achieving affordable critical care in low-income and middle- income countries. BMJ Global Health, 4(3), e001675.
11. Fukui, E. M., Lyons, P. G., Harris, E., McCune, E. K., Rojas, J. C., & Santhosh, L. (2023). Improving communication in intensive care unit to ward transitions: protocol for multisite national implementation of the ICU-PAUSE handoff tool. JMIR Research Protocols, 12(1), e40918.
12. Ghorbanzadeh, K., Ebadi, A., Hosseini, M., Madah, S. S. B., & Khankeh, H. (2021). Challenges of the patient transition process from the intensive care unit: a qualitative study. Acute and Critical Care, 36(2), 133.
13. Upadhyay, S., Stephenson, A. L., & Smith, D. G. (2019). Readmission rates and their impact on hospital financial performance: a study of Washington hospitals. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 56, 0046958019860386.
14. Endeshaw, A. S., Fekede, M. S., Gesso, A. S., Aligaz, E. M., & Aweke, S. (2023). Survival status and predictors of mortality among patients admitted to surgical intensive care units of Addis Ababa governmental hospitals, Ethiopia: a multicenter retrospective cohort study. Frontiers in Medicine, 9, 1085932.
15. Smith, Z. A., Ayele, Y., & McDonald, P. (2013). Outcomes in critical care delivery at jimma university specialised hospital, Ethiopia. Anaesthesia and intensive care, 41(3), 363-368.
16. smith-et-al-2013-outcomes-in-critical-care-delivery-at- jimma-university-specialised-hospital-ethiopia.
17. Yin, Y. L., Sun, M. R., Zhang, K., Chen, Y. H., Zhang, J., Zhang, S. K., ... & Hu, Z. J. (2023). Status and risk factors in patients requiring unplanned intensive care unit readmission within 48 hours: a retrospective propensity-matched study in China. Risk Management and Healthcare Policy, 383-391.
18. Mohammadi, S. S., Shafipour, V., Yazdani, C. J., & Heidari, G. M. A. (2019). Readmission to Intensive Care Unit: Frequency, Causes and Related Factors, International Journal of Pharmaceutical and Phytopharmacological Research. 2019.
19. Kaben, A., Corrêa, F., Reinhart, K., Settmacher, U., Gummert, J., Kalff, R., & Sakr, Y. (2008). Readmission to a surgical intensive care unit: incidence, outcome and risk factors. Critical care, 12, 1-12.
20. Rosenberg, A. L., & Watts, C. (2000). Patients readmitted to ICUs: a systematic review of risk factors and outcomes. Chest, 118(2), 492-502.