Research Article - (2025) Volume 3, Issue 1
Evaluating the Effect of Hyssopus Officinalis and Verbascum Thapsus Herbal Tea on SPO2 and Duration of Hospitalization in Patients With Covid-19
2Molecular and Medicine Research Center, Khomein University of Medical Sciences, Khomein, Iran
3Instructor, Department of Nursing Education, Khomein University of Medical Sciences, Khomein, Iran
4Traditional and Complementary Medicine Research Center (TCMRC), Department of Traditional Medicine, , IR Iran
Received Date: Mar 05, 2025 / Accepted Date: Apr 11, 2025 / Published Date: Apr 16, 2025
Copyright: ©©2025 Mr. Mohammad Taheri, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Taheri, M., Azizi, M., Salehi, M. (2025). Evaluating the Effect of Hyssopus Officinalis and Verbascum Thapsus Herbal Tea on SPO2 And Duration of Hospitalization in Patients with Covid-19. J Future Med Healthcare Innovation, 3(1), 01-09.
Abstract
Background: Due to Hyssopus Officinalis and Verbascum Thapsus’s anti-inflammatory and antiviral properties, they can be effective in accelerating the recovery process of patients with COVID-19. The purpose of this study was to investigate the effect of Hyssopus Officinalis and Verbascum Thapsus herbal tea on SPO2 and duration of hospitalization in hospitalized patients with COVID-19.
Materials and Methods: The present triple-blinded randomized clinical trial was conducted on 80 COVID-19 patients, using the simple randomization method in treatment and control groups. Patients in the treatment groups received Hyssopus Officinalis and Verbascum Thapsus herbal tea three times a day for 9 days, while patients in the control group received placebo black tea. SPO2 of patients was measured before and after the treatment every day and recorded in the checklists. Finally, SPO2 level and duration of hospitalization were compared using Stata-17 software.
Results: There was no statistically significant difference between the two groups before the treatment in SPO2 and baseline characteristics. No significant differences in SPO2 were observed between the two groups on the first day after the start of the treatment, while SPO2 was significantly higher in the treatment group from day 2 afterward (P<0.05). On average, patients in the treatment group were discharged 2.14 days earlier than patients in the control group (P=0.041).
Conclusion: Results showed that Hyssopus Officinalis and Verbascum Thapsus herbal tea could improve SPO2 and reduce the duration of hospitalization in hospitalized patients with COVID-19, and this herbal tea may be used for this disease.
Keywords
Hyssopus Officinalis, Verbascum Thapsus, SPO2, Duration of Hospitalization, COVID-19
Introduction
The COVID-19 pandemic caused by SARS-CoV-2 has challenged human beings as an invisible opponent [1,2]. COVID-19 was first reported in Wuhan, China, in 2019 and spread all over the world in a few months due to its high contagiousness causing more than 2 million deaths in the first 12 months of the pandemic and more
than 224 million definite cases and 4.6 million deaths until mid- September 2021 [3,4]. The manifestations of COVID-19 range from asymptomatic infection to life-threatening pneumonia [5]. The most common symptoms include coryza symptoms and acute respiratory distress syndrome [6]. The symptoms of COVID-19 mainly involve the respiratory system, which can be alleviated using complementary medicine [2].
According to the strategy of the World Health Organization (2014-2023), traditional medicine has many positive points and its application is expanding rapidly also according to the strategy of the White House, the National Center For Complementary and Alternative Medicine (NCCAM) has allocated most of the research budgets due to the importance of complementary medicine and is expanding the use of this branch of medicine in America and the world [7,8].
Using over-the-counter herbal compounds is an approach to complementary medicine for disease prevention and treatment [9]. The use of complementary medicine varies among countries, e.g., 34% in the United States and more than 50% in East Asia countries [10]. Complementary medicine presents an effective recommendation as a popular medicine with a holistic and comprehensive perspective for the prevention and treatment of diseases, even contagious diseases such as cholera and tuberculosis in the past and COVID-19 in the present [11].
Hyssopus Oficinalis is a fragrant self-growing plant in Europe, Asia Minor, and Iran. It has small, narrow, pointed, and symmetrical leaves on the stem, and the flowers are dense and spike-shaped at the end of the stem. This plant is used in traditional medicine for sore throat, cold, and hoarseness. Some herbalists believe that this plant has beneficial effects on asthma and swelling and inflammation of the urinary tract [12]. The anti-HIV effects of hyssop leaf extract have been seen. The important compounds of this plant include pinocamphon, isopinocamphon, alpha and beta-pinene, camphene, alpha terpenes, hisopine glucosides, hesperidin, and diosmin [13].
In preclinical studies, anti-microbial, anti-inflammatory, and expectorant effects have been shown. Ma et al. (2014) indicated in vivo use of Hyssopus Oficinalis extract regulated the levels of serums eosinophil in bronchoalveolar fluid and immunoglobulin IgG and IgE. Hyssopus Oficinalis also affects immune regulation. Tijana MiÃÂ??oviÃÂ?? et al. (2022) study indicated the anti-inflammatory activity of Hyssopus Oficinalis (in vitro and in vivo), that significant inhibitory activity was shown in the COX-2 test regarding extracts [14,15]. Ma et al have confirmed the anti- inflammatory and immune regulation role of hyssopus oficinalis in mouse with chronic asthma [15]. Its anti-inflammatory effect has been reported in an in-vivo study even more than NSAID referees [14]. Its antiviral property has also been proven in in-vivo studies [16].
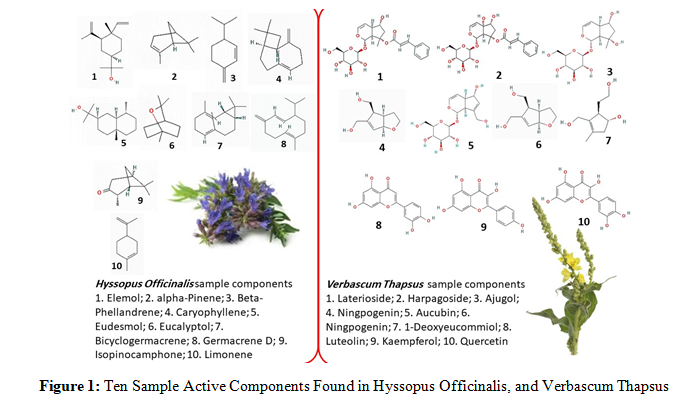
Verbascum Thapsus, mainly known as Khargoshak in Iran, has long been used in complementary medicine in many countries. It shows anti-microbial, anti-viral, anti-inflammatory, and antioxidant properties and is used to treat a wide range of diseases, including inflammatory disease of the respiratory system [17]. In addition to the many benefits considered for this plant in traditional medicine, the antiviral and anti-inflammatory effects of this plant has been confirmed in several in vitro and animal studies. The anti-inflammatory and antiviral effects of Verbascum Thapsus are due to the presence of the metabolite Isoliquiritigenin, which was reported in Sanger,s study on the medicinal metabolites of Verbascum Thapsus [18]. Its antiviral properties have also been confirmed under laboratory conditions on viruses such as influenza [19]. The biological effects of Hyssopus Oficinalis, and Verbascum Thapsus could be related to their various active components that Figure 1 depicts 10 examples of their active components.
The present study aims to investigate the effect of Hyssopus Oficinalis and Verbascum Thapsus herbal tea on SPO2 and duration of hospitalization in hospitalized patients with COVID-19.
Materials and Methods
Study Design
The present triple-blinded randomized clinical trial was conducted in the COVID-19 ward of Imam Khomeini Hospital of Khomein City in Markazi Province (located in the center of Iran) in 2020, which is the only hospital in Khomein admitting patients with COVID-19.
Participants’ Inclusion and Exclusion Criteria
The study participants were patients with COVID-19 referred to Imam Khomeini Hospital of Khomein. The study inclusion criteria were age above 18 years, consciousness, lack of oral nutrition contraindication and swallowing ability (for a daily drink of herbal tea), positive PCR test results, hospital admission, lung involvement in chest CT scan, presenting disease symptoms (fever, sore throat, dysphonia, dyspnea, cough, chest pain, and myalgia) classified as a moderate disease and having the consent to participate in the study. The exclusion criteria were unwillingness to continue the study, disease worsening and patient transfer to ICU, systolic blood pressure above 16 mmHg during the treatment, allergy to the herbal tea, underlying diseases such as cardiovascular disease, renal disease, hepatic disease, diabetes, pregnancy, and breastfeeding.
Sample Size and Sampling Method
The sample size was determined to be 40 patients in each group, considering the error of 5% and the power of 80% [20]. Convenient sampling was done from January 2020 to March 2020, considering the study inclusion criteria. Patients fulfilling the eligibility criteria were divided into treatment and control groups using simple randomization with a two-sided coin. Patients were assigned to the treatment group in case of tails and the control group in case of heads.
The study was designed as triple-blind, so that the patients, the treatment staff members (nurses and physicians), and the data analyzers did not know how patients were allocated to the study groups.
After allocating each person to one of the groups, the main researcher delivered one of the treatment or placebo bottles to each patient. From there, the numbers on the bottles were randomly written three-digit numbers, and the allocation of the patients remained blind.
Treatment Development
To prepare the herbal tea, fresh Hyssopus Oficinalis’s flowers, and Verbascum Thapsus’s leaves were handpicked from the mountain area and confirmed by a traditional medicine specialist. The collected herbs were washed, and the flower of Hyssopus Oficinalis and the leaves of Verbascum Thapsus were dried using the traditional method in a sanitary way under the sunlight. The herbal tea preparation was supervised by a traditional medicine specialist. A combination of 15 grams of Hyssopus Oficinalis flower and 5 grams of Verbascum Thapsus leaves were boiled for 20 min in 0.5 Liter of water, which was packed in 250 ml bottles after being cooled. The placebo herbal tea (black tea) was prepared with the same color and packed in the same bottles using pale black tea. Three-digit numbers were written on the bottles for concealment. The main researcher was aware of the content of the bottle and was not involved in the examinations and outcome measurement.
After obtaining permission to conduct the study and the ethics code from the research ethics committee of Khomein University of Medical Sciences, the eligible patients were selected from the patients admitted to hospitals. The study objectives were explained to them, and they were ensured of the confidentiality of the personal and clinical data and informed written consent was taken. Patients in the treatment groups received 250 ml of Hyssopus Oficinalis and Verbascum Thapsus herbal tea three times a day for 9 days, while patients in the control group received 250 ml of placebo herbal tea (black tea). Participants, nurses, physicians, and data analyzers were not aware of the bottle contents.
Patients in both groups received routine care in the hospital, in- cluding dexamethasone, enoxaparin, remdesivir, and pantoprazole in similar doses and using oxygen by nasal cannula or simple face mask. Each patient in the treatment group was matched with a pa- tient in control group considering the type of oxygen reception device. Note that a traditional medicine specialist was available during the study to control the potential side effects of the herbal tea.
The present study was approved by the research ethics committee of Khomein University of Medical Sciences with the ethics code of IR.KHOMEIN.REC.1399.012 and registered in the Iranian Registry of Clinical Trials with the registration code of IRCT20100130003227N15.
Measures
Outcome Measures
The outcomes in the present study include SPO2 measurement and hospitalization duration. SPO2 was measured using a pulse- oximeter (Wellex A310). The patient’s index finger was placed in the device, and after 30 sec, the SPO2 was recorded. SPO2 shows the hemoglobin oxygen saturation (Normal range: 94-99%). The hospitalization duration was recorded in days in the checklist of the patient’s clinical symptoms.
Assessment Tool
The assessment tool in this study included demographic information (Age, Sex, Education level, Job, and marital status) and the clinical symptoms checklist (Fever, myalgia, sore throat, dysphonia, dyspnea, cough, and chest pain), which was completed by trained individuals during the treatment for each patient.
Data Analysis
The collected data was analyzed in Stata-17 software. The two groups (treatment and control) were compared before the treatment in terms of baseline characteristics (age, sex, marital status, job, education level, drug history, onset-to-hospitalization) and SPO2 using chi-square and independent samples t-test. Repeated measures analysis was used to compare the changes in mean SPO2 in the treatment and control group during the treatment at α = 0.05.
A simple linear regression model at α = 0.2 was used to investigate the difference between the two groups in terms of duration of hospitalization. To measure the confounding of baseline characteristics, each of them was separately analyzed using multiple linear regression models at α = 0.2, and variables with significant relationships were considered as confounders which were used in the final model at α = 0.05. Regarding the analysis of the differences between the two groups in SPO2 at the end of the treatment, baseline characteristics and the confounding effect of pre-treatment SPO2 were investigated.
Results
Participants’ Characteristics
Table 1 summarizes the characteristics of the study participants. The mean age of participants in the control and treatment groups were and years, respectively. Most participants in both groups were female, married, illiterate, and housekeepers. Mean onset- to-hospitalization time was higher in the treatment group than in the control group, though no significant differences were observed between the two groups in terms of baseline characteristics (Table 1).
|
Variables |
Control group (n = 40) |
Treatment group (n = 40) |
|
Gender (No (%))a |
||
|
Female |
21 (52.5) |
21 (52.5) |
|
Male |
19 (47.5) |
19 (47.5) |
|
Marital status (No (%))a |
||
|
Single |
7 (17.5) |
5 (12.5) |
|
Married |
33 (82.5) |
33 (82.5) |
|
Divorced |
0 (0) |
2 (5) |
|
Job (No (%))a |
||
|
Employee |
15 (37.5) |
12 (30) |
|
Farmer |
5 (12.5) |
10 (25) |
|
Housewife |
18 (45) |
16 (40) |
|
Others |
2 (5) |
2 (5) |
|
Education level (No (%))a |
||
|
Illiterate |
13 (32.5) |
12 (30) |
|
Primary |
4 (10) |
2 (5) |
|
Middle |
11 (27.5) |
4 (10) |
|
Diploma |
4 (10) |
11 (27.5) |
|
Bachelor |
8 (20) |
11 (27.5) |
|
Drug History (No (%))a |
||
|
Dexamethasone, Remdesivir, Enoxaparin and Pantoprazole |
27 (67.5) |
26 (65) |
|
Dexamethasone, Enoxaparin and Pantoprazole |
13 (32.5) |
14 (35) |
|
Age (mean ± sd)b |
48.98±1.76 |
48.48±15.57 |
|
Onset-to-hospitalization time (mean ± sd)b |
8.95±4.40 |
9.30±4.39 |
Table 1: Baseline Characteristics of Participants in the Treatment and Control Groups
Changing of Mean SPO2 Scores in Treatment and Control Groups During the Study
Mean SPO2 in the control group was before the treatment, which was not significantly changed during the treatment (P = 0.142). Mean SPO2 in the treatment group was before the treatment, which showed a growing trend during the treatment reaching at the end of the study showing a statistically significant difference (P = 0.0001). Comparing means of SPO2 between the two groups showed no significant difference before the treatment and on the first day after the start of the treatment, though a significant difference persisted from the second day after the start of the treatment to the end of the study, and the SPO2 was significantly higher on the treatment group compared with the control group (Table 2).
|
Out- come |
Groups |
Before the treatment |
After the treatment |
P-Val- ue a |
||||||||
|
|
|
|
Day 1 |
Day 2 |
Day 3 |
Day 4 |
Day 5 |
Day 6 |
Day 7 |
Day 8 |
Day 9 |
|
|
SPO2% |
Control (Range) |
86.32 ± 7.71 (65-95) |
86.25 ± 8.43 (60-95) |
87.77 ± 6.07 (71-95) |
88.77 ± 5.77 (75-95) |
89.47 ± 5.34 (75-95) |
90.30 ± 4.59 (76-95) |
90.47 ± 4.48 (77-95) |
88.72 ± 10.04 (50-95) |
88.90 ± 9.92 (50-95) |
89.05 ± 10.25 (48-95) |
0.142 |
|
Treat- ment (Range) |
89.85 ± 6.03 (70-95) |
90.1 ± 5.87 (70-95) |
91.45 ± 5.00 (73-95) |
91.40 ± 4.93 (73-95) |
92.30 ± 4.34 (75-95) |
92.35 ± 4.33 (75-95) |
92.45 ± 3.92 (77-95) |
92.50 ± 3.72 (78-95) |
92.60 ± 3.33 (80-95) |
92.60 ± 3.33 (80-95) |
0.0001 |
|
|
P-Val- ue b |
|
0.026 |
0.020 |
0.004 |
0.032 |
0.011 |
0.044 |
0.040 |
0.029 |
0.028 |
0.041 |
|
|
a Sphericity Assumed Repeated Measures |
||||||||||||
Table 2: Evaluation of the Change in SPO2 Scores of Participants in the Study by Groups
Comparison of Mean SPO2 and Duration of Hospitalization Scores Between Treatment And Control Groups
Mean SPO2 was 6.57% higher in the treatment group than in the control group in the unadjusted mode, which reached 5.08% after adjustment for the confounder variables (P= 0.037). While no significant differences were observed in terms of duration of hospitalization in the unadjusted model, it was 2.14 days shorter in the treatment group compared with the control group after adjustment of the confounder variables (P = 0.041) (Table 3).
|
|
Unadjusted models a |
Adjusted models b |
|||||
|
Outcomes |
Coefficient |
80% CI |
P-Value |
Coefficient |
95% CI |
P-Value |
|
|
SPO2 |
Control group |
Reference |
|
|
|
|
|
|
Treatment group |
6.57 |
3.23, 9.91 |
0.013 |
5.08c |
0.311, 9.85 |
0.037 |
|
|
Duration of hospitalization |
Control group |
Reference |
|
|
|
|
|
|
Treatment group |
-1.25 |
-2.50, 0.006 |
0.202 |
-2.14d |
-4.19, -0.08 |
0.041 |
|
|
a Linear regression at α = 0.2 |
|||||||
Table 3: The Effect of the Treatment on the Mean Of Final SPO2 and Duration of Hospitalization Scores of Participants
Discussion
Currently, viral infections such as COVID-19 are the leading cause of morbidity and mortality all over the world, while no effective therapeutic approach has been developed for the management of COVID-19, and no anti-viral therapy has shown confirmed clinical effects [21-23]. A considerable amount of evidence suggests the anti-viral potential of some herbs [22]. The present study aimed to investigate the effect of Hyssop and Mullein herbal tea on the SPO2 and duration of hospitalization in hospitalized patients with COVID-19. During the treatment, the SPO2 of the patients in both groups was measured every day. No significant differences in SPO2 were observed between the two groups before the treatment and on the first day after the treatment, while SPO2 was significantly higher in the treatment group compared with the control group from day 2 afterward. Moreover, no significant differences were found in terms of SPO2 before the treatment and at the end of the treatment in the control group, whereas the SPO2 was significantly improved in the treatment group.
The duration of hospitalization in the treatment group was 1.25 days less than patients in the control group, although the difference was not statistically significant in the unadjusted model; though, the adjusted model considered confounders of age, education level, onset-to-hospitalization, and drug history, showed a significant difference. This effect was attributed to the anti-inflammatory and anti-viral effects of Hyssop and Mullein [24-26]. Hyssop has anti-cough, expectorant, and anti-inflammatory effects and thus has been used for a long in traditional medicine in patients with inflammatory processes [27]. The anti-inflammatory effects of Hyssop were evaluated in Micovic et al.’s study, in which it showed superior anti-inflammatory effects compared with NSAIDs such as indomethacin and ibuprofen [14].
Another study evaluated Hyssop’s effects on chronic obstructive pulmonary disease (COPD), which showed improved respiratory effects such as SaO2 and, finally, the quality of life of patients with COPD (20). Moreover, the positive effects of Hyssop on the symptoms of allergic rhinitis and cough in previous studies. With the onset of the COVID-19 pandemic and lack of definitive treatment and effective vaccines in the first days on the one hand and the strong background of traditional medicine and complementary medicine in the recovery of the viral infections of the respiratory system and the availability of low-cost herbs for the general population, on the other hand, several studies have investigated the effect of traditional medicine on different aspects of the disease in the recent years. For instance, Khorshiddost et al. conducted a clinical trial to investigate the effects of herbs containing Hyssop and some other plants and showed that they could facilitate COVID-19 recovery and reduce its undesired effects due to its anti-viral, anti-inflammatory, and immune system boosting [28-30].
Mullein flower also shows anti-inflammatory, antioxidant, anti- microbial, and anti-viral effects [19,31]. Polysaccharides and saponin in the Mullein flower play a pivotal role in the immune and anti-inflammatory effects [32,33]. The bioactive agents in the leaves and flowers of this plant are used in the treatment of various respiratory diseases such as whooping cough, dry cough, and asthma. Mullein extract is also used as an anti-inflammatory remedy for allergic diseases and pneumonia [34]. Results of a review article demonstrated the beneficial effects of the Mullein flower in bronchitis which may reduce the risks associated with the influenza virus [35]. Pal et al. investigated the effect of herbal chemicals in the prevention of COVID-19 and showed that anti- viral herbs such as Mullein flower could be the only choice for COVID-19 prevention in countries with high population density, which slows down vaccination [36].
Hyssop and Mullein show anti-inflammatory and anti-viral effects. The combination of these two herbs may intensity these effects, which explains the findings of the present study. Thus, it can be concluded that the traditional medicine and herbs, with proven effects in the previous study and historically used in disease treatment, are very helpful as complementary medicine in the COVID-19 pandemic. Recent databases showed an increasing number of studies on herbs in the COVID-19 pandemic. Thus, traditional herbs may start a new season in the study of new anti- viral agents [37].
Mechanism of Effect
In Figure 2 we have proposed a mechanism of action of herbal components that results in alleviation of tissue damage by COVID-19 infection. Cytokine release, and severe inflammatory responses in COVID-19 is associate with reactive oxygen spices (ROS) production, moderate and severe tissue damage. Further, in respiration distress and difficulty, the load of free radicals is increased due to the inflammatory process. Consequently, a tiny part of oxygen is expenditure for production of ROS. Hence, addition of antioxidants is expected to be beneficial in removing free radicals and limiting the tissue damage.
Insilco studies, and clinical or laboratories findings confirm the benefits of usage of medicinal plants in controlling inflammatory responses. Components found in medicinal plants may have pharmacologic effects on metabolic and molecular signaling pathways, in addition to their antioxidation characteristics. A suspected mechanism of action of herbal ingredients is the blockade of inflammatory enzymes such as prostaglandin synthase-2 that produces inflammatory cytokines, as shown previously by one of our research team members. For example, cacao usage by diabetic patients reduces the inflammatory markers, mediators and cytokines (hs-CRP, TNF, IL-6, Malondialdehyde) [38].
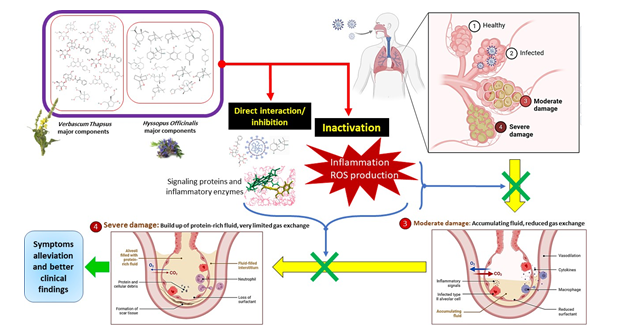
Figure 2: Proposed Mechanism of Action Of Active Components of Hyssopus Oficinalis, and Verbascum Thapsus in Alleviating of Clinical Findings in Treatment Group
Overall, in Figure 2 we considered at least two methods of action for phytochemicals found in Hyssopus Oficinalis and Verbascum Thapsus tea (Figure 1): 1) inactivation of ROS agents by their antioxidant properties, and 2) direct interaction with, and consequently inhibition of viral and signaling proteins or inflammatory enzymes. We think that better oxygen saturation occurred in that patients treated with a tea containing phytochemicals with antioxidant and pharmacologic agents than patients only received oxygen.
Conclusion
Results of the present study showed that Hyssopus Oficinalis and Verbascum Thapsus herbal tea (250 ml three times a day) increases SPO2 and reduces the duration of hospitalization in the treatment group compared with the control group, while no side effects were reported. Yet, considering the limited number of studies in this regard, further confirmatory studies are required. Given the anti-inflammatory effects of Hyssopus Oficinalis and Verbascum Thapsus, it is suggested to conduct further studies on other inflammatory diseases of the respiratory system. The participants of the present study were aged above 18 years, and the effects of this herbal tea were not investigated in patients aged below 18 years, which may be addressed in future studies.
List of Abbreviations
There is no abbreviation
Declarations
Statement of Ethics: All the ethical considerations based on the international ethical protocols were considered by the authors and the work was approved by the ethics committee of the Khomein of Medical Sciences University (Approval code: IR.KHOMEIN. REC.1399.012). This study has also been registered in the Iranian Registry of Clinical Trials (IRCT20100130003227N15).
Consent for Publication
Written informed consent was obtained from the patients to publish this article and any accompanying images. A copy of the written consent is available for review by the journal's Editor-in-Chief.
Data Availability Statement:
Please contact the corresponding author (Mohammad Taheri) for data requests.
Conflict of Interest Statement:
The authors have no conflicts of interest to declare.
Funding Sources:
Not applicable.
Authors' contributions:
Mohammad Taheri proposed the original concept and designed the treatment and collected data. Mohammad Taheri and Mehdi Salehi prepared the herbal tea. Mohammad Taheri and Mahdieh Azizi, equally participated in the data analysis. All authors contributed to writing the manuscript.
Acknowledgments:
We would like to thank all the staff of Imam Khomeini Hospital in Khomein city, especially the patients with Covid-19 disease who helped us in this study.
References
1. Ng, J. Y. (2020). Global research trends at the intersection of coronavirus disease 2019 (COVID-19) and traditional, integrative, and complementary and alternative medicine: a bibliometric analysis. BMC complementary medicine and therapies, 20, 1-9.
2. Sarkar, P. K., & Mukhopadhyay, C. D. (2022). Mechanistic insights from the review and evaluation of ayurvedic herbal medicines for the prevention and management of COVID-19 patients. Journal of Herbal Medicine, 32, 100554.
3. Pepera, G., Tribali, M. S., Batalik, L., Petrov, I., & Papathanasiou, J. (2022). Epidemiology, risk factors and prognosis of cardiovascular disease in the Coronavirus Disease 2019 (COVID-19) pandemic era: a systematic review. Reviews in cardiovascular medicine, 23(1), 28.
4. Pan, L., Wang, J., Wang, X., Ji, J. S., Ye, D., Shen, J., ... & Wang, L. (2022). Prevention and control of coronavirus disease 2019 (COVID-19) in public places. Environmental Pollution, 292, 118273.
5. Struyf, T., Deeks, J. J., Dinnes, J., Takwoingi, Y., Davenport, C., Leeflang, M. M., ... & Cochrane COVID-19 Diagnostic Test Accuracy Group. (2022). Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVIDâ?19. Cochrane database of systematic reviews, (5).
6. Zahmatkesh, S., Klemeš, J. J., Bokhari, A., Wang, C., Sillanpaa, M., Hasan, M., & Amesho, K. T. (2022). Critical role of Hyssop plant in the possible transmission of SARS- CoV-2 in contaminated human Feces and its implications for the prevention of the virus spread in sewage. Chemosphere, 305, 135247.
7. WHO traditional medicine strategy: 2014-2023.
8. DuÈ?u, L. E., Popescu, M. L., Purdel, C. N., Ilie, E. I., LuÈ?Ä?, E. A., Costea, L., & Gîrd, C. E. (2022). Traditional medicinal plants—a possible source of antibacterial activity on respiratory diseases induced by chlamydia pneumoniae, haemophilus influenzae, klebsiella pneumoniae and moraxella catarrhalis. Diversity, 14(2), 145.
9. Wieland, L. S., Piechotta, V., Feinberg, T., Ludeman, E., Hutton, B., Kanji, S., ... & Garritty, C. (2021). Elderberry for prevention and treatment of viral respiratory illnesses: A systematic review. BMC complementary medicine and therapies, 21, 1-15.
10. Mulder, L. T., Busch, M., Kristoffersen, A. E., Hök Nordberg, J., & van der Werf, E. T. (2022). Prevalence and predictive factors of complementary medicine use during the first wave of the COVID-19 pandemic of 2020 in the Netherlands. BMC Complementary Medicine and Therapies, 22(1), 43.
11. Shirazi, M. T., Karimi, M., Masoom, S. M. F., Mardi, R., Kamyabnezhad, M. M., & Eghbalian, F. (2021). COVID-19 Telephone Consultation by Iranian Traditional Medicine as an Integrative Medicine: Benefits and Challenges. Traditional and Integrative Medicine.
12. Hyssop. Review of Natural Products. factsandcomparisons4.0 [online]. 2005. Available from Wolters Kluwer Health, Inc. Accessed April 17, 2007.
13. Norouzi, R., Adnani Sadati, J., Yaghoubian, R., Mirzaei, F., Fateh, R., & Siadatpanah, A. (2021). Evaluation of antitrichomonal effect of methanolic extract of Hyssopus officinalis on Trichomonas vaginalis in vitro. Qom University of Medical Sciences Journal, 14(12), 14-21.
14. MiÄ?oviÄ?, T., StankoviÄ?, J. S. K., Bauer, R., Nöst, X., MarkoviÄ?, Z., MilenkoviÄ?, D., ... & MaksimoviÄ?, Z. (2022). In vitro, in vivo and in silico evaluation of the anti-inflammatory potential of Hyssopus officinalis L. subsp. aristatus (Godr.) Nyman (Lamiaceae). Journal of Ethnopharmacology, 293, 115201.
15. Ma, X., Ma, X., Ma, Z., Sun, Z., Yu, W., Wang, J., ... & Ding, J. (2014). The effects of uygur herb Hyssopus officinalis
L. on the process of airway remodeling in asthmatic mice. Evidenceâ?Based Complementary and Alternative Medicine, 2014(1), 710870.
16. Sharifi-Rad, J., Quispe, C., Kumar, M., Akram, M., Amin, M., Iqbal, M., ... & Cho, W. C. (2022). Hyssopus essential oil: an update of its phytochemistry, biological activities, and safety profile. Oxidative Medicine and Cellular Longevity, 2022(1), 8442734.
17. Taleb, S., Ozgoli, G., Mojab, F., Nsiri, M., & Ahvazi, M. (2016). Effect of Verbascum Thapsus cream on intensity of episiotomy pain in primiparous women. The Iranian Journal of Obstetrics, Gynecology and Infertility, 19(7), 9-17.
18. Sanger, E. (2022). Medicinally Useful Metabolites Of Common Mullein Endophytes.
19. Riaz, M., Zia-Ul-Haq, M., & Jaafar, H. Z. (2013). Common mullein, pharmacological and chemical aspects. Revista brasileira de farmacognosia, 23(6), 948-959.
20. Abdolahinia, A., Naseri, M., Eslaminejad, A., Ghaffari, F., & Velayati, A. (2018). Effect of Nepeta bracteata benth. on chronic obstructive pulmonary disease: a triple-blinded, randomized clinical trial. Iranian Red Crescent Medical Journal, 20(12), e80112
21. Abou Baker, D. H., Amarowicz, R., Kandeil, A., Ali, M. A., & Ibrahim, E. A. (2021). Antiviral activity of Lavandula angustifolia L. and Salvia officinalis L. essential oils against avian influenza H5N1 virus. Journal of Agriculture and Food Research, 4, 100135.
22. Saberâ?Moghaddam, N., Salari, S., Hejazi, S., Amini, M., Taherzadeh, Z., Eslami, S., ... & Elyasi, S. (2021). Oral nanoâ?curcumin formulation efficacy in management of mild to moderate hospitalized coronavirus diseaseâ?19 patients: An open label nonrandomized clinical trial. Phytotherapy research, 35(5), 2616-2623.
23. Abd-Elsalam, S., Salama, M., Soliman, S., Naguib, A. M., Ibrahim, I. S., Torky, M., ... & Elhendawy, M. (2021). Remdesivir efficacy in COVID-19 treatment: a randomized controlled trial. The American Journal of Tropical Medicine and Hygiene, 106(3), 886.
24. Pirnia, M., Shirani, K., Yazdi, F. T., Moratazavi, S. A., & Mohebbi, M. (2022). Characterization of antioxidant active biopolymer bilayer film based on gelatin-frankincense incorporated with ascorbic acid and Hyssopus officinalis essential oil. Food Chemistry: X, 14, 100300.
25. Babich, O., Sukhikh, S., Prosekov, A., Asyakina, L., & Ivanova, S. (2020). Medicinal plants to strengthen immunity during a pandemic. Pharmaceuticals, 13(10), 313.
26. Dalar, A., Guo, Y., & Konczak, I. (2014). Phenolic composition and potential anti-inflammatory properties of Verbascum cheiranthifolium var. cheiranthifolium leaf. Journal of Herbal Medicine, 4(4), 195-200.
27. Sadr, S., Kaveh, N., Agin, K., Choopani, R., Kaveh, S., & Tahermohammadi, H. (2022). Herbal treatments for Asthma, according to Avicenna. Journal of Pediatric Perspectives, 10(1), 15205-15226.
28. Hajiheydari, M. R., Yarmohammadi, M. E., Izadi, P., Jafari, F., Emadi, F., Emaratkar, E., ... & Naseri, M. (2017). Effect of Nepeta bracteata Benth. on allergic rhinitis symptoms: A randomized double-blind clinical trial. Journal of Research in Medical Sciences, 22(1), 128.
29. Sehar, N., Alam, M. I., Ahmad, S. A. T., Ahmad, M. W., & Goswami, A. (2015). Clinical study of unani formulation ‘Sharbat Zoofa Murakkab’in the management of sual ratab (productive cough). Hippocratic J Unani Med, 10(3), 1-8.
30. Khorshiddoust, R. R., Khorshiddoust, S. R., Hosseinabadi, T., Mottaghitalab, F., Mokhtari, F., Azadinia, F., ... & Mohammadian, A. (2022). Efficacy of a multiple-indication antiviral herbal drug (Saliravira®) for COVID-19 outpatients: A pre-clinical and randomized clinical trial study. Biomedicine & Pharmacotherapy, 149, 112729.
31. Panchal, M. A., Murti, K., & Lambole, V. (2010). Pharmacological properties of Verbascum thapsus—A review. Int J Pharm Sci Rev Res, 5(2), 73-77.
32. Akdemir, Z., Kahraman, Ç., Tatlı, I. I., Akkol, E. K., Süntar, I., & Keles, H. (2011). Bioassay-guided isolation of anti- inflammatory, antinociceptive and wound healer glycosides from the flowers of Verbascum mucronatum Lam. Journal of ethnopharmacology, 136(3), 436-443.
33. Sohrabi-Haghdost, R. V., & Safarmashaei, S. (2011). Comparison of in-vivo wound healing activity of Verbascum thapsus flower extract with zinc oxide on experimental wound model in rabbits. Advances in Environmental Biology, 5(7), 1501-9.
34. Shahbaz, F., Akhter, N., Shahid , M., Riaz, M., Anjum, F., & Hussain, F. (2022). Ultrasound assisted extraction and characterization of bioactives from v erbascum thapsus roots to evaluate their antioxidant and medicinal potential. Dose- Response, 20(2), 15593258221097665.
35. Abiri, R., Abdul-Hamid, H., Sytar, O., Abiri, R., Bezerra de Almeida Jr, E., Sharma, S. K., ... & Malik, S. (2021). A brief overview of potential treatments for viral diseases using natural plant compounds: The case of SARS-CoV. Molecules, 26(13), 3868.
36. Pal, S., Chowdhury, T., Paria, K., Manna, S., Parveen, S., Singh, M., ... & Mandal, S. M. (2022). Brief survey on phytochemicals to prevent COVID-19. Journal of the Indian Chemical Society, 99(1), 100244.
37. Roy, P., Pramanick, K., Das, A., Majumdar, M., Roy, A., & Sarkar, U. (2022). Review of Some Herbal Agents Having Antiviral Activity. International Journal of Current Science Research and Review, 5(3), 695-706.
38. Parsaeyan, N., Mozaffari-Khosravi, H., Absalan, A., & Mozayan, M. R. (2014). Beneficial effects of cocoa on lipid peroxidation and inflammatory markers in type 2 diabetic patients and investigation of probable interactions of cocoa active ingredients with prostaglandin synthase-2 (PTGS- 2/COX-2) using virtual analysis. Journal of diabetes & metabolic disorders, 13, 1-9.