Case Report - (2024) Volume 9, Issue 2
Case Study: Impact of Pelvic Floor Muscle and Yoga Training on Improving Three Women Uterine Prolapse
Received Date: May 31, 2024 / Accepted Date: Jul 02, 2024 / Published Date: Jul 08, 2024
Copyright: ©©2024 Najwa Alfarra. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Alfarra, N. (2024). Case Study: Impact of Pelvic Floor Muscle and Yoga Training on Improving Three Women Uterine Prolapse. Int J Womenâ??s Health Care, 9(2), 01-16.
Abstract
Background: The incident of pelvic organ prolapses (POP) is 25% to greater than 90%. The symptoms of uterine prolapse can be extremely debilitating and impact patient’s quality of life [1]. This is a common problem in aging women. Main symptoms of POP are vaginal heaviness and discomfort, especially during sexual intercourse, in addition to urinary incontinence [2]. Physiotherapy is qualified as a conservative treatment to improve the tone and strength of the pelvic floor muscles through specific exercises and yoga techniques for the pelvic floor muscles to promote greater support for the pelvic viscera [3]. These techniques can improve the symptoms in mild and moderate cases and prevent the pelvic organs from slipping down further [4]. Aim of the Study: To explore the effectiveness of Yoga poses and Kegel exercises as a way of preventing and treating pelvic organ prolapse.
Case Description: Three women were referred to Physical Rehabilitation department by the Obstetrics and Gynecology physician. The first participant is 38 years old of age presented with a history of heaviness and discomfort in the vagina and pelvic pressure for one year. Urgency present sometimes, had one child. Had restricted physical activities such as standing up, walking, aerobic classes Second informant was a 45 years old had a history of six months heaviness at the lower abdominal area and discomfort in the vagina, had restricted physical activities such as walking, standing, jumping, running and aerobic classes and tensing up with anticipation of sex, unable to carry her baby, because the symptoms will get worse, and a companied with occasional stress incontinence, had three children, the last participant was 46 years old with a history of five years of stress incontinence and heaviness in the vagina, restricted her from doing housework and carrying her child. It requires her to manually push deeper the protruding organ and to empty the bowel easily, had chronic constipation, and had five children.
Management and Outcomes: Three participants received yoga training and Kegel exercises once per week for eight weeks in the clinic, followed by unsupervised (phone follow up )Kegel exercises and Yoga poses at home program for four weeks (12 sessions). After the completion of fourth weeks, they were seen at the clinic for reassessment and discharge. Outcomes as suggested by Hagen, et al, which included pre/post Pelvic Organ Prolapse-symptoms score (POP-ss), followed by prolapsed uterus symptoms, pelvic organ prolapse impact questionnaire, and the clinician’s observations.
Result: Significant effects in prolapsed uterus and urinary incontinence were reported following supported Yoga training and Kegel exercises program by two participants with significant improvement from the baseline to week 12. While third participant moderately improved in prolapsed uterus grade and almost cured stress incontinence.
Conclusion: Yoga poses and Kegel exercises program intended to address the pelvic floor and core muscles were found to have better outcomes in terms of decreasing prolapsed uterus and stress incontinence.
Keywords
Pelvic Organ Prolapse, Physical Therapy, Pelvic Floor Exercises, Yoga for Pelvic Floor
Introduction
Uterine prolapse is a health concern affecting millions of women worldwide. When it defined by symptoms has prevalence of 3-6% and up to 50% when based upon vaginal examination [5]. It defined as a condition in which the pelvic floor organs move partially or completely from their normal position and move towards the genital hiatus, because of weakness and /or stretching of the muscles and ligaments that act in the support of these organs [3]. The etiology of POP in women: vaginal delivery, a large baby, forceps, or vacuum-assisted birth, prolonged or very quick second stage of labor and having multiple deliveries increase the risk of prolapse. Lacerations stretching of tissues, and tearing of the perineum can also affect pelvic floor integrity and damage nerves. Certain health conditions such as chronic cough, chronic straining due to constipation, obesity and connective tissue disorders [6]. Pelvic organ prolapse is categorized in four stages, ranging from mild to severe. In mild cases, women may be totally unaware that something has shifted until their gynecologist discovers it during a routine pelvic examination. In addition , pelvic organ prolapse quantification system graded POP as follows; stage (0) no prolapse is demonstrated, stage (I) the most distal portion of the prolapse is more than 1 cm above the level of the hymen, stage (II) the most distal portion of the prolapse is a 1 cm or less proximal or distal to the hymen, stage (III) the most distal portion of the prolapse protrudes more than 1 cm below the hymen but no farther than 2 cm less than the total vaginal length, and stage (IV) vaginal eversion is essential complete [4].
Women with POP commonly have a variety of symptoms including pelvic heaviness, dragging sensation in the vagina, protrusion coming down from the vagina, and backache. Bladder and bowel symptoms, discomfort during sexual intercourse are also frequently present. In women with mild or moderate POP do not experience any of theses symptoms until any aspect of the vaginal wall actually protrudes beyond the opening of the vagina [7]. treatment options for prolapse depend on the severity of the symptoms; mild to moderate prolapse is usually treated with conservative methods such as physical therapy modalities. More sever prolapse often needs surgery [7]. Physical therapy intervention is essential in both prevention and detection of prolapse, but very few literatures evaluate physical therapy intervention for the treatment of patients with POP [8].
Methodology
• Design: Case study of three women will be utilized to fulfill the aim of this study.
• Setting: The study will be conducted at physical rehabilitation affiliated to King Faisal specialist hospital
• Sample: Three women will be recruited in the study according to the inclusion criteria.
• Inclusion Criteria: Age group ranged from 35-50 years, Educated women (bachelor degree). Women who clinically diagnosed as uterine prolapse 1st and 2nd Degree. With/without stress incontinence, Multipara women.
• Exclusion Criteria: Women with reproductive tract infection and urinary tract infection or any other gynecological complications. Women with 3rd and 4th Degree uterine prolapse
Method
• Design: Case study of three women will be utilized to fulfill the aim of this study.
• Setting: The study will be conducted at physical rehabilitation affiliated to King Faisal specialist hospital
• Sample: Three women will be recruited in the study according to the inclusion criteria.
• Inclusion Criteria: Age group ranged from 35-50 years, Educated women (bachelor degree). Women who clinically diagnosed as uterine prolapse 1st and 2nd Degree. With/without stress incontinence, Multipara women.
• Exclusion Criteria: Women with reproductive tract infection and urinary tract infection or any other gynecological complications. Women with 3rd and 4th Degree uterine prolapse
Interviewing Phase
The researcher held the first interview with each woman in the outpatient physical rehabilitation clinic during the physical therapy first session, oral consent for participation in the study was obtained from selected women for ethical issues and scheduled times and frequency of sessions and follow up, mobile phone numbers were saved to all selected women to assure adherence to the intervention.
Implementation phase
The researcher conducted the educational sessions about Kegel exercises and yoga poses for the participants in this study. The total number of Kegel exercises and yoga poses training sessions was one session/week through 8 weeks. duration for each session was ranged from 20 to 30 minutes. Followed by phoned calls every week for another 4 weeks, to find out if they were regularly performing the exercises and have any other problems facing them to determine degree of her compliance with the Kegel yoga poses at home and checked women progress. Total of 12 sessions (8 sessions physical attendance, and 4 phon calls sessions).
The First Session
Took about 45 minutes and at the beginning of this session, the researcher introduces herself, explained the objective of the research, gave them an educational booklet about Kegel exercises and Yoga poses, then illustrated the content of the booklet; through gave the women simple information about anatomy of the female reproductive system, anatomy of the female pelvis, and anatomy of pelvic floor muscles, and assessed the patient.
Case Description
This study is limited to three participants. The participants of this study were given a coded name, when indicating their results see Table 1
Table 1
|
Participant 1 |
Participant 2 |
Participant 3 |
|
P1 |
P2 |
P3 |
Patients History
Patient 1 (P1)
First participant was 38 years old with complains of POP with urgency after first vaginal delivery. The patient diagnosed with POP after Ob. Gynecology examination.
• Obstetric-Gynecologist History: Had one vaginal delivery, had polycystic ovarian disease, and one miscarriage
• Labor Complications: Prolonged first stage of labor during delivery, and episiotomy.
• Chief Complains: The patient experienced heaviness and discomfort in the vagina, pelvic pressure. It causes anxiety, fear and avoidance of sexual activity. She had to restrict physical activities, such as stand up for long time, aerobic exercises, running, jumping, dancing and walking for more than half an hour. One child. Urgency present sometimes. No prior history of Physical Therapy intervention or medication.
• Aggravating Factors: Prolonged standing, heavy lifting, walking, constipation, weight gain.
• Relieving Factors: Rest, Lying Down
Patient 2 (P2)
The second participant was 45 years old complained of POP last six months. Shortly after her third vaginal delivery. The patient was diagnosed with POP and occasionally stress incontinence during a postpartum examination and referred to physical therapy clinic.
• Obstetric-Gynecologist History: Vaginal delivery x 3 and one miscarriage. Tried different pessaries, none of the pessaries stayed well in desired positions
• Labor Complications: Prolonged second stage of labor during last delivery, episiotomy, and 1st. degree perineal tear
• Chief Complaints: The patient experienced heaviness at the lower abdominal area , and discomfort in the vagina, it caused mood disturbance, irritation, and anger she had to restrict physical activities such as walking, standing, running, jumping, aerobic classes and tensing up with anticipation of sex” since the onset of her symptoms. Unable to carry her child, because of the symptoms will be worse. Constipation will worsen her condition as well. Had three children. No prior history of Physical Therapy intervention or medication.
• Aggravating Factors: Prolonged standing, carrying her child, walking, constipation.
• Relieving Factors: Rest, lying down or sitting.
Patient 3 (P3)
The last participant was 46 years old with a history of stress incontinence and POP shortly after her fifth vaginal delivery and diagnosed with POP after OB. Gynecology examination Obstetric-gynecologist history: vaginal delivery x 5.
• Labor Complications: Prolonged first stage of labor during fourth delivery, episiotomy, and 2nd degree perineal tear.
• Chief Complaints: The patient experience heaviness in the vagina, while she is cooking, and get worse with carrying her child and stand up. It required the patient to manually push deeper the protruding organ to be able to empty the bowel. Had chronic constipation. She had to restrict walking, aerobic exercises or stand up to cook or clean the house. No other medical history presented.
• Aggravating Factors: Prolonged standing, carrying her child, walking, constipation.
• Relieving Factors: Rest, lying down.
Table 2: Characteristic of the Participants
|
Characteristic |
P1 |
P2 |
P3 |
|
Age |
38 Y/O |
45 Y/O |
46 Y/O |
|
Education |
Bachelor degree |
Bachelor degree |
Bachelor degree |
|
Occupation |
Teacher |
Teacher |
Lab technician |
|
Marital status |
Married |
Married |
Married |
|
Length of time with prolapsed uterus |
1 year |
6 months |
5 years |
|
Self-report severity |
Mild |
Moderate |
Moderate |
|
Constipation |
None |
Sometimes |
Always |
|
Menopause |
No |
No |
No |
|
No. of children |
1 |
3 |
5 |
|
Type of delivery |
Normal |
Normal |
Normal |
|
BMI |
23.5 |
24 |
24.5 |
The data collection for this study was conducted in March 2024, where the researcher met the participants in the physical rehabilitation department, interviewed them and explained the benefits of Kegel exercises and Yoga training program. Obviously, all participant’s ultimate goal with PT is to get better and cured from prolapsed uterus and stress incontinence. At the beginning of treatment, the authored discussed with each one of them the short-term, long-term goals and explained to them the period it will take to achieve the short-term versus long-term goals.
Evaluation Phase
Evaluation phase was done at pre-intervention as a base data and after 6 weeks and 3 months.
Assessmet
Table 3: Observation/External Examination
|
Muscle palpation: Check the connective tissue elasticity for the following muscles: |
P1 |
P2 |
P3 |
|
1-Abdomen and suprapubic area |
Normal |
Normal |
Normal |
|
2-Pelvis,Labia, Perineum area, through groin area, ischial tuberosity (IT), and anterior through suprapubic |
Minimal restriction. |
Minimal restriction. |
Minimal restriction. |
|
External Muscular Assessment: Trigger points |
Normal |
Normal |
Normal |
|
Visual inspection of Vulva/Vestibule/Pelvic Floor Muscle: |
The perineal reflex and anal wink were normal, |
The perineal reflex and anal wink were normal, |
The perineal reflex and anal wink were normal, |
|
Prolapsed uterus grade |
Grade 1 |
Grade 11 |
Grade 11 |
|
Types of the prolapse |
Anterior |
Anterior |
Anterior |
|
Continence |
Rarely |
Occasionally |
Sometimes |
Internal Examination
Internal Pelvic Floor Muscle Assessment Tone is minimally increased globally in all participants.Connective tissue lateral to urethra and urethral sphincter were normal in all participants Prolapsed uterus grade one in P1, while P2 and P3 grade 2. Trigger points: No trigger points at all the participants.
Table 4: Specific Measurement of the Pelvic Floor Muscles
|
Measurement |
P1 |
P2 |
P3 |
|
Muscle power |
2/5 |
2/5 |
2/5 |
|
Endurance |
4/10 |
3/10 |
3/10 |
|
Repetition |
6/10 |
3/10 |
3/10 |
|
Fast contraction |
5/10 |
2/10 |
4/10 |
Findings
Minimally increase tone and shortening of the pelvic floor muscles in all participants. Pelvic floor muscles strength, endurance, repetition and fast contraction was decreased as shown at table 4 in all participants. All the participants had different prolonged stage of delivery with episiotomy with/without perineal tear. All the participants were unable to stand up, carry heavy things or walk for long time. This situation prevented them from aerobic exercises such as jumping; running dancing or walk for more than half an hour, as well as they avoided sexual activity and some of them unable to stand up to do the house work.
Second session: took about 30 minutes: the researcher gave the participants a detailed demonstration about Yoga poses and Kegel
exercises program and helps the participants to identify the correct pelvic floor muscles for the training. Treatment included:
1. Pranayama (Breathing Exercises):
• Ask the patient to take deep breath from the nose the hands on chest and abdominal should raises up during the inhale process.
• Then exhale from mouth the hands on chest and abdominal should go down, repeat 3-4 times.
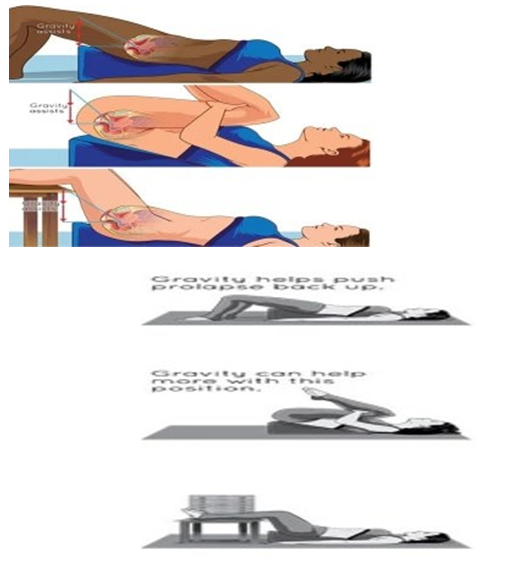
Resting Pose and Perform Kegel exercise from that Position.
• Ask the patient to lay down and raise the hips with a wedge, this position will help the patient to contract and feel the pelvic floor
muscles working.
• Ask the patient to contract pelvic floor muscles count up to 4 se. relax and count up to 4 sec. repeat 4-5 times.
• Stay in that position for 10 min. once/day
Uttanapadasana (One Leg Poses)
• From supine position. Patient will raise one leg to 90 degree and hold for 10-15 seconds while breathing normally. Slowly lower the leg. Repeat 2-3 times, with both legs.
• The same routine will also be used at 60 and 45 degrees from the floor

Naukasana (Boat pose)
• The patient will raise legs, arms, shoulders and head off the ground, as shown in the picture. Squeeze the abdominal and pelvic floor muscles up but breathe normally in the posture.
• Hold for 10-15 seconds at least. Repeat 2-3 times.

Kandharasana (Shoulder Pose)
• The patient will Bend knees, keeping the feet apart on the floor. Then will lift the hips up and tighten the gluteus muscles. Rise as high as possible, pushing the chest up towards the chin, but keep feet flat on the floor.
• Hold the posture for as long as it is comfortable and then lower the body to the starting position. Repeat 2-3
Mula Bandha (Downward-Facing Dog):
• Ask the patient to bend the head and shoulders toward the floor, drawing the hips away from hands, and lifting and spreading the sitting
bones.
• Hold for 10-15 seconds at least. Repeat 2-3 times

Outcomes
The author adopted:
1. Pelvic Organ Prolapse symptoms score (POP-ss), by Hagen, et al [6]. which include: seven items relating to the frequency of prolapse symptoms in the previous weeks and after completed the sessions of treatment,
2. Women perceived change in prolapse symptoms since the start of the treatment (same, better, worse).
3. Pelvic organ prolapses impact questionnaire.
4. The clinician’s observations (anatomical and functional).
All the participants answered the Pelvic Organ Prolapse symptoms score (POP-ss), Arabic validated version by the Egyptian Journal of hospital medicine and Patient reported prolapsed symptoms change before commencement and upon completion of the treatment [9].
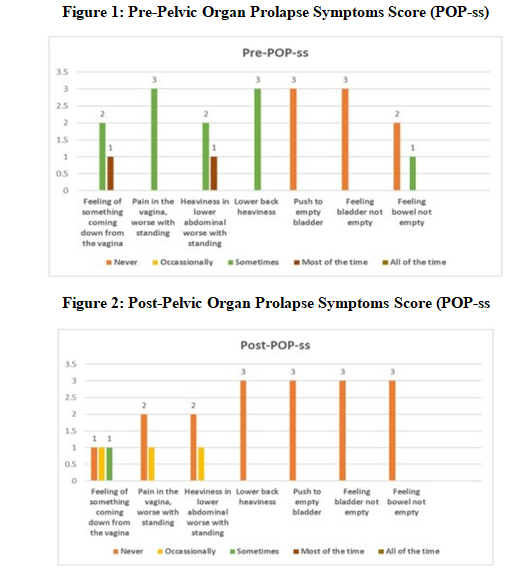
There were a significant improvement regarding to uterine prolapse- symptoms post-intervention compared to pre-intervention, Table 5.
Table 5: Change in Prolapsed Symptoms
|
Degree of uterine prolapse symptoms |
Pre- intervention |
Post-6 weeks intervention |
Post- 3 months intervention |
|
Nile |
|
|
1 |
|
Mild |
1 |
1 |
2 |
|
Moderate |
2 |
2 |
|
|
Severe |
|
|
|
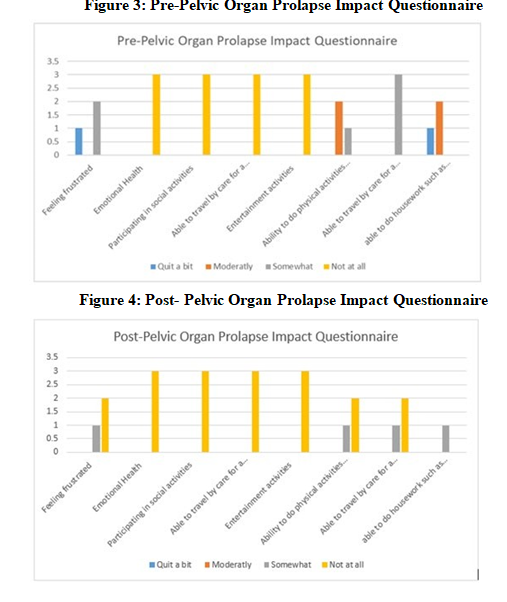
It reveals that there was a highly difference between Pre- Pelvic organ prolapse impact questionnaire compared to post- intervention, Figure 3&4.
The result illustrated relationship between yoga poses and Kegel exercises with uterine prolapse self-report, and pelvic floor muscles
strength and endurance. It was noticed that there was improvement Table 5.
Table 5: Comparison of Pelvic Floor Muscles Strength and Endurance / Uterine Prolapse Self-Report and Incontinence Before and After the Intervention
|
Measurement |
P1-Pre Rx. |
P1-Post Rx. |
P2- Pre Rx. |
P2- Post Rx. |
P3- Pre Rx. |
P3- Post Rx. |
|
Muscle power |
2/5 |
3/5 |
2/5 |
3/5 |
2/5 |
3/5 |
|
Endurance |
4/10 |
6/10 |
3/10 |
6/10 |
3/10 |
6/10 |
|
Repetition |
6/10 |
8/10 |
3/10 |
8/10 |
3/10 |
7/10 |
|
Fast contraction |
5/10 |
7/10 |
2/10 |
7/10 |
4/10 |
7/10 |
|
Uterine prolapse patients (self- report) |
Mild |
Not at all |
Moderate |
Mild |
Moderate |
Mild |
|
Incontinence |
Some times |
Rarely |
Occasionally |
Never |
Sometimes |
Occasionally |
After 6 weeks, the author assessed the following changes: P1 was able to perform aerobic exercises twice per week, walk for half an hour without pain, and able to reach bathroom without leakage of urine, with full bladder. No pain with sexual activity. P2 was able to return to normal sexual activity, and started aerobic classes for half an hour, and able to carry her child and stand for half an hour without pain. P3 was able to hold urine leakage during sneezing if the bladder was full, able to cook and do house activity with minor pain and she had to take a rest in between, sexually active.
After 12 sessions, the authors re-assess the participants: P1 was able to go back to her normal activity pain free and cured incontinence, no bulging symptoms. P2 able to do aerobic exercises once/week for one hour free of pain with limitation to jumping and running activity to eliminate bulging symptoms, normal sexual relationship, able to stand up and carry her child for long time pain free. P3 able to do house work free of pain, decrease in constipation/straining during bowel movements, able to do aerobic exercises for half an hour free of pain , no bulging symptoms once/ week. All participants confirmed that their lifestyle changed with Yoga that resulted in weight loss.
Discussion
The aim of this study was to assess the effect of Kegel exercises and yoga training on improving manifestations of uterine prolapse among three women. Findings of the current study showed that all the studied women were multipara and had normal vaginal deliveries this is may be due to among parous women the odd for symptomatic pelvic organ prolapse increased with a number of childbirths. That goes with Bijalwan et al confirmed this finding and reported that pelvic organ prolapse is a common health problem affecting nearby 40%of multipara women above 34 years of age [10]. Moreover, the current study findings revealed that there was a relationship between demographic characteristics with uterine prolapse symptoms. It was noticed that there was a highly significant relation between the women's uterine prolapse symptoms with their age, educational status and their occupation. These findings reflected that the educated and workable women may had source of information about risk factors for uterine prolapse including vaginal childbirth, advancing age, more births and they tried to avoid these factors. In relation to this result, several epidemiological studies as Dumoulin, Hay-Smith who studied Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women; they have the similar finding when examined the association between uterine prolapse symptoms and stages and participant characteristics such as age, education, and parity [11]. These factors were theoretically hypothesized as significant confounders of POP this comparable between younger and older participant educated, non- educated.
The study confirmed that the women who followed Kegel exercises and yoga training program would have improvement in manifestations of uterine prolapse and urinary incontinence. This finding agreed with those of Berzuk, et al, who studied randomized controlled trial on efficacy of pelvic floor muscle training for treating pelvic organ prolapse and urinary incontinence in women, who had POP with incontinence their age was more than 40 years [12]. Furthermore, as regards to uterine prolapse symptoms, the current study findings displayed that, there were significant improvement of prolapse staging post intervention after 3 months, and confirmed that the women who follow Kegel exercises and yoga training showed less symptoms than before. In accordance with a finding Priyanka, et al, reported that, the intensity of symptoms of POP reduced after 4 months of intervention [13]. Moreover, McClurge, et al suggested that pelvic floor exercises help to improve a mild prolapse and related symptoms [14]. Pelvic floor muscle training resulted in significant anatomic improvement of anterior and posterior vaginal wall prolapse and better muscle strength.
Regarding compliance to performance of Kegel exercises and Yoga poses training program, the current study results displayed that nearly one participant was moderate compliance compared with the relation between other two participants compliance to performance Kegel exercises and yoga training with uterine prolapse symptoms after 1 and 3 months. These findings reflected that the adherence to performing exercises daily help increase its effect and may make it on time is usual and increase women self-efficacy to perform which increase PFM strength. This study findings were in the same line with a recent randomized controlled trial to intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence; a randomized comparative trial by Felicissimo, found that commitment to PFMT was as effective for women with POP and increases their compliance and exercise adherence, which lead to successful effect [15].
Moreover, it was observed that there was significant relation between problems resulting in increasing pressure in abdomen with uterine prolapse degree of symptoms. This may be regarded to that there is evidence that a vaginal delivery, and increased abdominal pressure significantly weakens and stretches the pelvic floor muscles and increase susceptibility to uterine prolapse. These findings supported by Shrestha, et.al, who found in their study majority of respondents (81.3%) increasing pressure on abdomen and carrying heavy loads as causes of uterine prolapse and increase its symptoms [16]. Moreover, it was, observed that there was a highly statistically significant relation between uterine prolapse degree of symptoms with gravidity and parity at (P value ≤ 0.001). As over the last few years, there has been increasing interest in the role of levator ani-muscle injuries in the development of uterine prolapse; there was relation between levator ani defects and uterine prolapse; women with levator ani defects are at least twice as likely to show clinically significant uterine prolapse. Ani muscle strongly affected by women gravidity and parity. This result supported by Acharya, who studied Contributing Factors of Utero-vaginal Prolapse among Nepali Parous Women and Divya, et al who studied Knowledge Regarding Utero -vaginal Prolapse among Women in Sree Balaji Medical College and Hospital who reported that uterine prolapse strongly affected by mode of delivery and parity with statistical significance differences [17,18].
Conclusion and Recommendation
The current study findings concluded that Kegel exercises and yoga training program had been demonstrated to be effective in inducing significant improvement in manifestations of uterine prolapse among women. The practice of Yoga encourages healthy lifestyle, and made many lifestyle changes that resulted in weight loss, decrease in constipation/straining during bowel movements, better stress management and improved posture alignment. During follow –up visits, the participants pelvic floor muscles strengthening had objectively improved from 2/5 to 3/5. The particpants reported no bulging symptoms and has been able lead an active lifestyle [19-22].
Limitations of the Study
This case study is limited to observations recorded in three women. Because of benefits of Kegel exercises and yoga poses experienced by three participants, further research would be beneficial in establishing a link between the practice of specific techniques of yoga and control /reversal of pelvic floor issues. Randomized controlled clinical trials may be encouraged.
References
1. Streicher L., (2013). Uterine prolapse and relaxation gynecological specialist of northwestern. prolapse htm.
2. Mercier, J., Morin, M., Lemieux, M. C., Reichetzer, B., Khalifé, S., & Dumoulin, C. (2016). Pelvic floor muscles training to reduce symptoms and signs of vulvovaginal atrophy: a case study. Menopause, 23(7), 816-820.
3. Rodrigues, A. M., Oliveira, L. M. D., Martins, K. D. F., Roy, C. A. D., Sartori, M. G. F., Girão, M. J. B. C., & Castro, R. D. A. (2009). Risk factors for genital prolapse in a Brazilian population. Revista Brasileira de Ginecologia e Obstetrícia, 31, 17-21.
4. Elbiss, H. M., Osman, N., & Hammad, F. T. (2015). Prevalence, risk factors and severity of symptoms of pelvic organ prolapse among Emirati women. BMC urology, 15, 1-5.
5. Barber, M. D., & Maher, C. (2013). Epidemiology and outcome assessment of pelvic organ prolapse. International urogynecology journal, 24, 1783-1790.
6. Hagen, S., & Stark, D. (2008). Physiotherapists and prolapse: who's doing what, how and why. Journal of the Association of Chartered Physiotherapists in Women’s Health, 103, 5-11.
7. Culligan, P. J. (2012). Nonsurgical management of pelvic organ prolapse. Obstetrics & Gynecology, 119(4), 852-860.
8. Xavier, B. D., De, S. Ã., Josefa Nicole Arruda, G., & Daphne, G. (2021). Physiotherapy to Prevent and Treat Women with Uterine Prolapse. Biomedical Journal of Scientific & Technical Research, 35(3), 27617-27619.
9. The Egyptian Journal of hospital medicine (July, 2017).Vol. 68 (2); 1252-1256
10. Bijalwan, R. P., Bhagavatula, M., Semwal, V. D., Rawat, P., & Anand, V. (2015). Morbidity of uterine prolapsed among the women in the Chakrata block of Dehradun District. Indian Journal of Community Health, 27(1), 103-109.
11. Dumoulin C, Hay-Smith J. (2010): Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev Jan 20;(1): CD005654.
12. Berzuk, K., & Shay, B. (2015). Effect of increasing awareness of pelvic floor muscle function on pelvic floor dysfunction: a randomized controlled trial. International urogynecology journal, 26, 837-844.
13. Priyanka, Kaur, S., Singh, A., & Aggrawal, N. (2015). A Pre- experimental Study to assess the Effectiveness of Nursing Intervention Package on Management of Pelvic Organ Prolapse among Women. Nursing & Midwifery Research Journal, 11(3), 131-143.
14. McClurg, D., Hilton, P., Dolan, L., Monga, A., Hagen, S., Frawley, H., & Dickinson, L. (2014). Pelvic floor muscle training as an adjunct to prolapse surgery: a randomised feasibility study. International urogynecology journal, 25, 883-891.
15. Felicíssimo, M. F., Carneiro, M. M., Saleme, C. S., Pinto, R. Z., da Fonseca, A. M. R. M., & da Silva-Filho, A. L. (2010). Intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: a randomized comparative trial. International urogynecology journal, 21, 835-840.
16. Shrestha, B., Choulagai, B., Onta, S., Shrestha, K. B., Petzold, M., & Krettek, A. (2014). Knowledge, prevalence and treatment practices of uterine prolapse among women of reproductive age in the Jhaukhel-Duwakot Health Demographic Surveillance Site, Bhaktapur, Nepal. Journal of Kathmandu medical college, 3(4), 136-143.
17. Acharya, S., &Acharya, S. (2016). Contributing factors of utero- vaginal prolapse among Nepali parous women. International Journal of Nursing Research and Practice, 3(2).
18. Divya, H., & Sathiyalatha, S. (2015). Knowledge Regarding Utero-vaginal Prolapse among Women in Sree Balaji Medical College and Hospital, Chennai. Journal of Nursing and Health Science, 4(1).
19. El-Azab, A. S., Ghoniem, G. M., Leu, S. Y., & Nguyen, D. V. (2015). Arabic validation of the pelvic organ prolapse/ incontinence sexual questionnaire, IUGA-revised (PISQ- IR). International urogynecology journal, 26, 1229-1237.
20. Carramo Silvia (2009) Random study of surgical correction of uterine prolapse using a synthetic type 1 polypropylene mesh comparing hysterectomy versus uterine preservation. Rev. Col Bras Cir Rio de Janeiro 36 (1): 65-72.
21. Hoffman, B. L., Schorge, J. O., Bradshaw, K. D., Halvorson, L. M., Schaffer, J. I., & Corton, M. M. (Eds.). (2016). Williams gynecology (Vol. 25). New York: McGraw-Hill Education.
22. Persu, C., Chapple, C. R., Cauni, V., Gutue, S., & Geavlete, P. (2011). Pelvic Organ Prolapse Quantification System (POP– Q)–a new era in pelvic prolapse staging. Journal of medicine and life, 4(1), 75.
Appendix
First Tool: Part 1 General Characteristics
|
Socio-demographic characteristics |
Comments |
|
|
Age |
|
|
|
Educational level |
|
|
|
|
Read and write |
|
|
|
Primary |
|
|
|
Secondary |
|
|
|
University |
|
|
Marital status |
|
|
|
|
Married |
|
|
Divorced |
|
|
|
Widow |
|
|
|
Body Mass Index |
|
|
Appendix: 2
Part II: Obstetric and Gynecological History
|
Obstetrics and Gynecology |
Comments |
|
|
Parity |
|
|
|
|
No children |
|
|
Two times |
|
|
|
Three times |
|
|
|
Four times or more |
|
|
|
Mode of delivery |
|
|
|
|
Normal vaginal delivery |
|
|
Cesarean section |
|
|
|
Duration of pelvic organ prolapse (months) |
|
|
|
|
< 6 |
|
|
|
6 - 12 |
|
|
12 - 24 |
|
|
|
Stage of prolapse |
|
|
|
|
Stage I |
|
|
Stage II |
|
|
|
Stage III |
|
|
|
Type of prolapse |
|
|
|
|
Anterior |
|
|
Posterior |
|
|
|
Anterior and Posterior |
|
|
Appendix: 3
Part III: Women Knowledge about Pelvic Organ Prolapse
|
Knowledge about pelvic organ prolapse |
Before intervention |
After intervention |
||||
|
Completely correct answer |
Incomplete correct answer |
Don’t know |
Completely correct answer |
Incomplete correct answer |
Don’t know |
|
|
Meaning |
|
|
|
|
|
|
|
Types |
|
|
|
|
|
|
|
Causes |
|
|
|
|
|
|
|
Symptoms |
|
|
|
|
|
|
|
Diagnosis |
|
|
|
|
|
|
|
Complications |
|
|
|
|
|
|
|
Preventive measures |
|
|
|
|
|
|
|
Measures for relieving POP symptoms |
|
|
|
|
|
|
|
Treatment Options |
|
|
|
|
|
|
Appendix: 4
Second Tool: Women Compliance Toward Recommended Physiotherapy Instructions Sheet
|
Compliance Items |
After one month |
After three months |
||
|
Practicing the pelvic floor muscle exercise correctly and regularly |
|
|
||
|
|
|
Comply |
|
|
|
Sometimes |
|
|
||
|
Not comply |
|
|
||
|
Weight reduction |
|
|
||
|
|
Comply |
|
|
|
|
Sometimes |
|
|
||
|
Not comply |
|
|
||
|
Avoidance sitting in squatting position or standing for long hours |
|
|
||
|
|
Comply |
|
|
|
|
Sometimes |
|
|
||
|
Not comply |
|
|
||
|
Avoid lifting heavy things |
|
|
||
|
|
Comply |
|
|
|
|
Sometimes |
|
|
||
|
Not comply |
|
|
||
|
Intake food that contains fiber to avoid constipation |
|
|||
|
|
Comply |
|
|
|
|
Sometimes |
|
|
||
|
Not comply |
|
|
||
|
Avoidance of high impact activity/exercise |
|
|
||
|
|
Comply |
|
|
|
|
Sometimes |
|
|
||
|
Not comply |
|
|
||
Appendix: 4
Third Tool: Pelvic Organ Prolapse Symptoms Score (POP-SS
|
How often during the last four weeks have you had the following symptoms |
Never |
Occasionally |
Sometimes |
Most of the time |
|
|
Feeling of something coming down from the vagina |
|
|
|
|
|
|
Uncomfortable feeling or pain in the vagina which is worse when standing |
|
|
|
|
|
|
A heaviness or in your lower Abdominal increase when standing |
|
|
|
|
|
|
Lower back heaviness |
|
|
|
|
|
|
Push to empty bladder |
|
|
|
|
|
|
A feeling bladder not empty |
|
|
|
|
|
|
A feeling bowel not empty |
|
|
|
|
|
Appendix: 6
Fourth Tool: Pelvic Organ Prolapse Impact Questionnaire
|
Ability to do household chores such as cooking, laundry and housecleaning |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
Quite a bit |
|
|
Ability to do physical activities such as walking or other exercise |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
Quite a bit |
|
|
Entertainment activities such as going to a movie or concert |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
|
Quite a bit |
|
Ability to travel by car or bus for a distance more than 30 minutes away from home |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
Quite a bit |
|
|
Participating in social activities outside home |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
Quite a bit |
|
|
Emotional health (nervousness, depression) |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
Quite a bit |
|
|
Feeling frustrated |
|
|
|
Not at all |
|
Somewhat |
|
|
Moderately |
|
|
Quite a bit |
|


