Research Article - (2025) Volume 9, Issue 1
Assessment of Pharmacists Knowledge, Attitude and Practice of Male Partner Inclusion in Postnatal Pharmaceutical Care Delivery
2Department of Pharmaceutical Services, State House Medical Centre, Abuja FCT, Nigeria
3Independent Researcher, Abuja FCT, Nigeria
Received Date: Jan 04, 2025 / Accepted Date: Mar 11, 2025 / Published Date: Mar 25, 2025
Copyright: ©©2025 Bilkisu Mohammed Kuchazi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Kuchazi, B. M., Amlogu, A. M., and Ogugua, J. O. (2025). Assessment of Pharmacists Knowledge, Attitude and Practice of male partner inclusion in postnatal pharmaceutical care delivery. Archives of Infect Diseases & Therapy, 9(1), 01-20.
Abstract
The postnatal period is crucial to the lives of mother and child but remains the most neglected time for providing high quality treatment. Providing pharmaceutical care during the postnatal period offers valuable benefits for the health and well-being of both the mother and child. Involving male partners of nursing mothers in providing such care will create a beneficial synergy of care with positive results. This is attributed to the significance of male partners in households with nursing mothers, often serving as family heads, and the importance of pharmacists as crucial members of the healthcare system. Gathering insights on the knowledge, attitudes, and practices (KAP) of pharmacists concerning the inclusion of males’ partners in delivering pharmaceutical care to nursing mothers is crucial for formulating future health action strategies and plans.
A mixed method research was conducted. This included a cross-sectional study among 211 pharmacists working in hospital pharmacies using online google questionnaires. Complimentary qualitative research was conducted where 14 pharmacists were interviewed using in-depth semi-structured interviews. A correlation test was used for analysing KAP scores.
Results indicate pharmacists across all demographics have adequate comprehension of the benefits of male partner inclusion in postnatal pharmaceutical care delivery. Female pharmacists are skeptical about their ability to persuade men to get involved in care and are more interested in receiving additional training and development to provide care. Results also show variations in practice across all demographics attributable to the challenges faced by pharmacists in practice.
Continued professional development for pharmacists should include training on strategies for involving men in the pharmaceutical care delivery for postnatal patients. Policy makers should recognize the importance of compulsory inclusion of male partners in provision of such care.
Keywords
Pharmacy, Postnatal Pharmaceutical Care Delivery, Sexual and Reproductive Health (SRH)
Introduction
The postnatal period is a crucial time in the lives of mothers and new-borns. Enhancing the utilization of postnatal care is a global goal, aimed at reducing maternal mortality and enhancing maternal healthcare (Angore et al., 2018). Nevertheless, this period remains the most overlooked in terms of delivering high-quality treatment (WHO, 2013). Maternal mortality rate has remained high for two decades, with Nigeria country accounting for 20 % of global maternal deaths (Ope, 2020). Maternal and neonatal morbidity and mortality rates can be decreased by increasing the use of facility-based care for women and newborns in low-resource settings (Greenspan et al., 2019). Men hold the primary decision-making role in LMICs and exert significant influence on women's access to maternal health services and subsequently impacting their health outcomes (Yargawa and Leonardi-Bee, 2015). An article in Frontlines, a monthly publication of the United States Agency for International Development (USAID), referring to Millennium Development Goal 5 (MDG), stated that "reducing maternal deaths by 75 percent worldwide by 2015 will require the involvement of men in countries where it matters most" (USAID, 2010).
Pharmaceutical care prescribes that the pharmacist takes the time to analyse, create a care plan, and follow up on patients (Thomas, 2018). It entails collaboration between health care providers (including a clinical pharmacist) in planning, implementing, and monitoring a therapeutic plan with the patient, as well as patient education on their drugs and disease condition (Elnour et al., 2008). Inclusion of intimate partners of nursing mothers as part of postnatal pharmaceutical care plan will ensure compliance to drug therapy and enhance moral and psychological support to the mother during the rigorous postnatal period. This will invariably improve health outcomes, which is the crux of pharmaceutical care. Pharmaceutical Care is the pharmacist's contribution to patient care to maximize the use of medications and enhance medical results and provision of optimal pharmaceutical care improves patient outcomes (Elnour et al., 2008).
The World Health Organization (WHO) recommends that postnatal care encompasses the ensuring the timely discharge from a healthcare facility after childbirth (typically 24 hours after uncomplicated vaginal delivery), conducting postnatal follow- up contacts and home visits, assessing the well-being of both the mother and child, promoting exclusive breastfeeding, offering guidance on cord care, facilitating immunization, encouraging interactions like bathing and playing with the baby, providing counselling to the mother, administering iron and folic acid supplementation, offering prophylactic antibiotics, and delivering psychosocial support to prevent the development of postpartum depression (PPD) in vulnerable women (WHO, 2013). Postpartum spousal support will invariably improve maternal and child health and wellbeing, reduce post-partum depression, child neglect and abuse, and maternal abuse. Spousal support to the nursing mother is expected to improve compliance with drug therapy, fewer illness visits, reductions in hospitalization and generally improve health outcomes. This forms part of the fourth component of pharmaceutical care (Thomas, 2018).
Effective collaboration and communication between the pharmacist and male partners of nursing mothers is part of the pharmaceutical care plan that will invariably lead to enhancement of optimum care postpartum. It is imperative to assess pharmacists’ knowledge, attitude, and practice of male partner inclusion in the provision of postnatal pharmaceutical care delivery, as the success of such collaborative intervention depends on awareness, attitude, and adequate implementation by the pharmacists.
Methods
Study Design
This is a mixed-method study conducted on pharmacists practicing in the hospital and community pharmacy settings in Nigeria using a triangulation method comprising of both quantitative and qualitative research techniques.
Study Setting
A KAP survey model was employed whereby the use of in-depth interviews and questionnaires were employed simultaneously.
For the semi-structured interviews, a research pool of four hospital pharmacy departments across Abuja Municipal Area Council was created. The study was conducted among members of the sites from the research pool. The total number of pharmacists from the sites were fourteen (14). Interviews were done within a period of four (4) days. Pharmacists at the hospitals were invited to participate in the discussions through colleagues working at the various healthcare centers. These colleagues ranged from fellow pharmacists’, nurses, and porters. All respondents were practicing and fully registered pharmacists.
Study Instrument
The study was conducted using a twenty-eight (28) item KAP questionnaire, composed of four (4) sections. The questionnaire was developed following an extensive literature review. Questionnaires were developed following the WHO KAP survey template (WHO, 2008). Questionnaires were administered online to pharmacists working in primary, secondary, and tertiary health care centres in Nigeria. Focus group discussions were also employed, face-to-face dialogue carried out between the researcher and pharmacists were recorded and transcribed.
Sample Size
For the cross-sectional study, the Kish Leslie’s formula for sample size calculation was employed, 30% attrition was included. Sample size obtained was 211. For semi-structured interviews, a total number of pharmacists interviewed were fourteen (14).
Data Collection
For quantitative data, the study was conducted using online distribution of google forms. For qualitative data, a research pool of four hospital pharmacy departments across Abuja Municipal Area Council (AMAC) was created. The study was conducted among members of the sites from the research pool. Questionnaires were distributed online. Consent forms were distributed via direct administration to pharmacists who consented to participate and could spare few minutes of their time to engage an interview.
Inclusion and Exclusion Criteria
Pharmacists across Nigeria practicing in hospital and community pharmacies were included. Pharmacists in Nigeria practising outside clinical settings such as those strictly in academia, research, and development were excluded. Adults aged 25 or older were included.
Data Analysis: Descriptive statistics such as frequencies and percentages were calculated. Chi-square test was used to determine the level of association between variables. Inferential analysis was done using Microsoft Excel and IBM SPSS Statistical Software Version 23. Thematic analysis was employed for analysis of qualitative data.
Results
Demographic Data: A total of 211 respondents were enrolled for this study, consisting of males and females with age groups ranging from less than 25 to 46 years and above. The dominant age group was 25-35 (48.3 %), whilst male had the dominant gender of 53.1 %. Majority (40.3 %) of the participants had 11-20 years of experience with B.Pharm. qualification (46.4 %).
|
Variables |
Frequency (%) |
|
Age groups |
|
|
25 to 35 |
102 (48.3) |
|
36 to 45 |
90 (42.7) |
|
46 and above |
13 (6.2) |
|
Less than 25 |
6 (2.8) |
|
Gender of participant |
|
|
female |
99 (46.9) |
|
male |
112 (53.1) |
|
Years of experience |
|
|
11 to 20 |
85 (40.3) |
|
21 and above |
6 (2.8) |
|
5 to 10 |
60 (28.4) |
|
less than 5 |
60 (28.4) |
|
Qualification |
|
|
B. pharm |
98 (46.445) |
|
Pharm. D |
20 (9.47) |
|
Masters |
64 (30.33) |
|
PHD |
8 (3.79) |
|
FPC Pharm. |
21(9.95) |
Table 1: Demographic Data
Knowledge
More than half of the respondents are very aware of the importance of counselling postpartum patients and this category fall underage (0.47%) group 25 to 35 (39.34%) and 35 to 45 (39.81%). In addition, only are not aware of the importance.
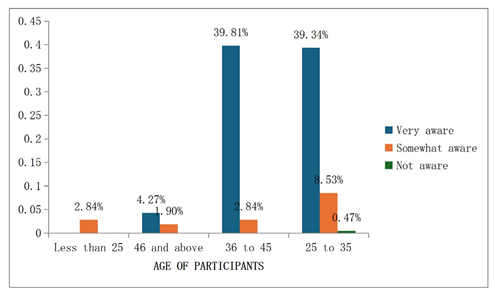
Figure 1: Relationship between age and Knowledge on Counselling about Medication adherence and Lifestyle Optimisation
99.53% of the respondents are very aware of the positive impact of intimate partner support on the physical and mental health of nursing mothers. Pharmacists within the age group 25 to 35 form the highest percentage (41.23%) of pharmacists who are fully “aware”.
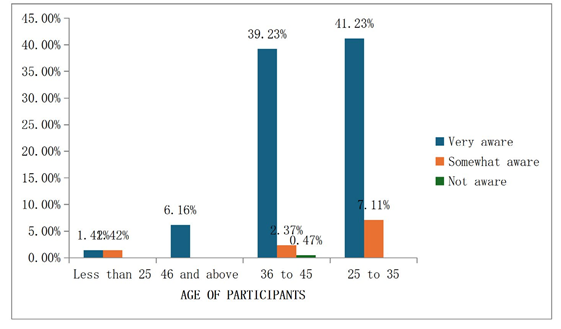
Figure 2: Relationship between Age and Knowledge on Impact of Partner Support on Physical and Mental Health
99.53% of the respondents are very aware that men should be targeted for inclusion in awareness programs. Pharmacists within the age group 36 to 45 form the highest percentage (38.86%) of pharmacists who are fully “aware”.
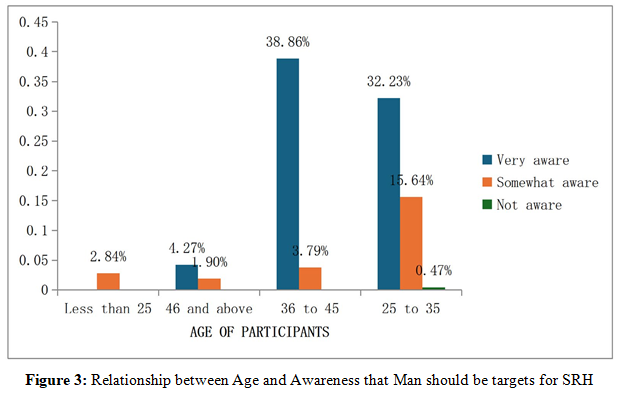
99.53% of respondents are knowledgeable of the benefits. The chart shows that 39.81% of pharmacists between the ages of 36 to 45 form
the majority of those who are “aware”.
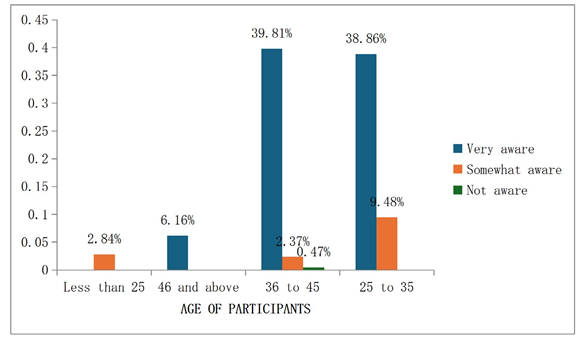
Figure 4: Relationship between Age and Knowledge on Benefits of Intimate Partner Participation in Care of Mother and Child 99.53% of all respondents have knowledge of these benefits. The dominant percentage score (38.86%) of participants falls under the age group of 36-45.

Figure 5: Relationship between Age and Knowledge on Benefits of Accompanying Women to Health Care Facilities during the Post- Natal Period
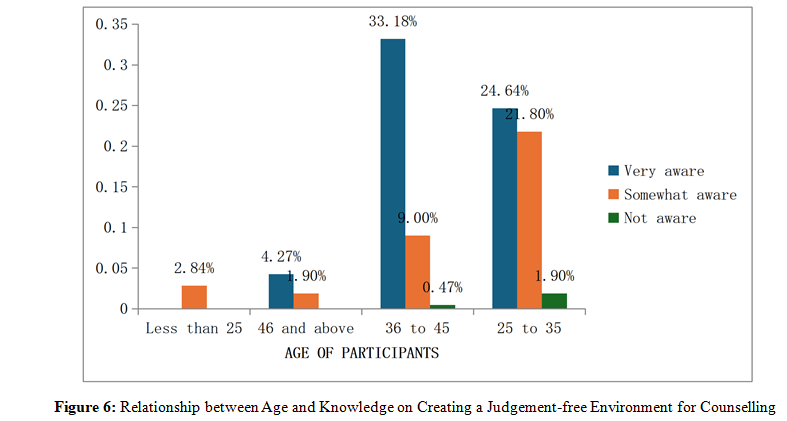
97.63% of all respondents are aware. The highest percentage score of aware participants is (33.18%) which is in the category of 36 to 45 years.
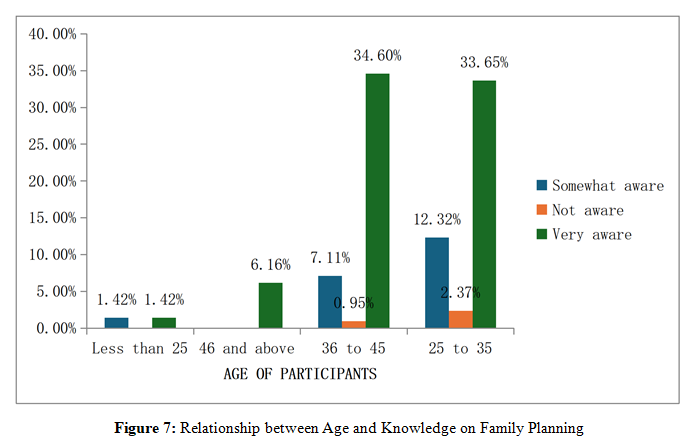
75.83% of all respondents are “very aware”, 20.85% are “somewhat aware” and 3.32% “not aware” to having knowledge on family planning. The dominant group that agrees has 34.60% with age range 36 to 45 and 33.65% with agree range 25 to 35.
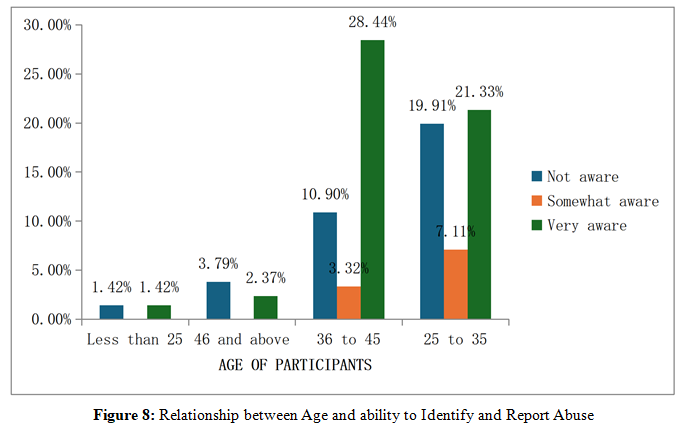
89.57% believe they have adequate knowledge to identify abuse and report it. 10.43% disagree. The dominant group that agrees has percentage score 28.44% and in the age range of 36 to 45.
The majority (99.53%) of respondents across all groups of professional qualification are aware of the importance of counselling in the current context with only (0.47%) not aware.
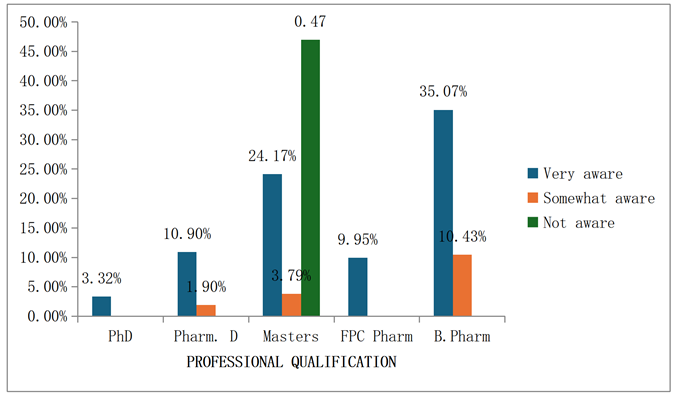
Figure 9: Relationship between Professional Qualification and Knowledge on Counselling About Medication Adherence and Lifestyle Optimisation
Majority (99.53%) of the respondents across all groups of professional qualification are aware of the importance of counselling in the current context with only a negligible percentage (0.47%) being unaware.
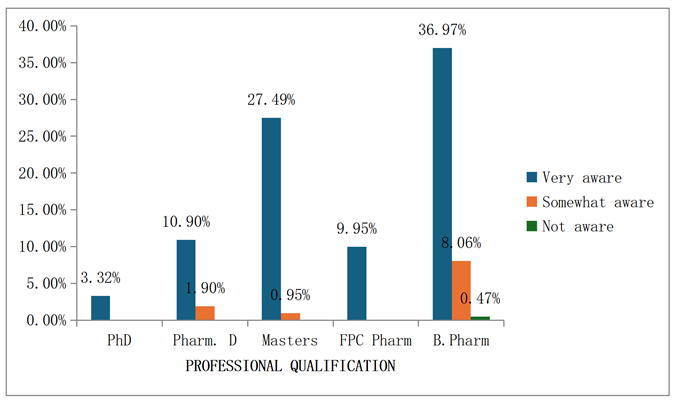
Figure 10: Relationship between Professional Qualification and Knowledge on Impact of Partners Support on Physical and Mental
Health of Mothers
96.68% of the respondents across all groups of professional qualification are aware that men should be targets for health education and awareness programs on sexual and reproductive health. 3.32% are not aware.

Figure 11: Relationship between Professional Qualification and Awareness That Man Should Be Targets for Health Education and Awareness Programs on SRH
99.53% of the respondents across all groups of professional qualification are aware of the of benefits of intimate partner participation in care of mother and child. 0.47% are not aware.
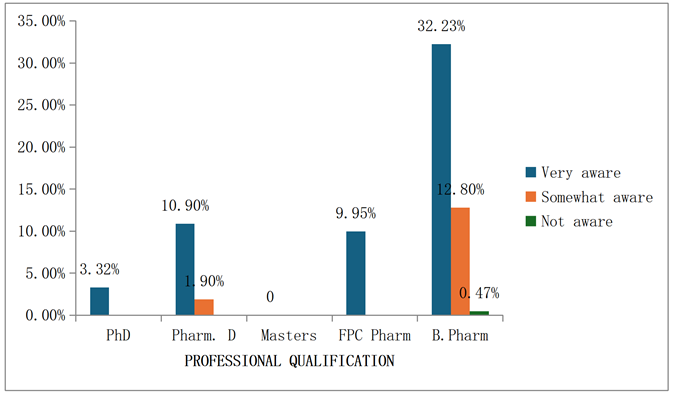
Figure 12: Relationship between Professional Qualification and Knowledge of Benefits of Intimate Partner Participation in Care of Mother and Child
99.53 % of the respondents across all groups of professional qualification are aware of the benefit of accompanying mothers to healthcare facilities. 0.47 % are not aware.
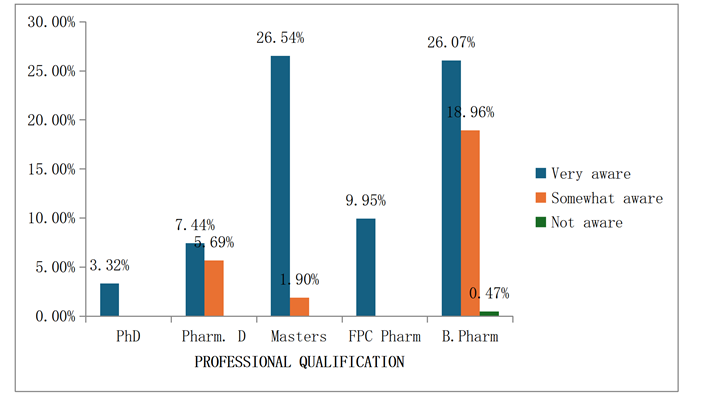
Figure 13: Relationship between Professional Qualification and Knowledge about Benefits of Accompanying Mothers to Healthcare Facilities
97.63% of the respondents across all groups of professional qualification are aware of the importance of creating a judgement- free environment for interaction with male partners of nursing mothers. 2.37% are not aware.
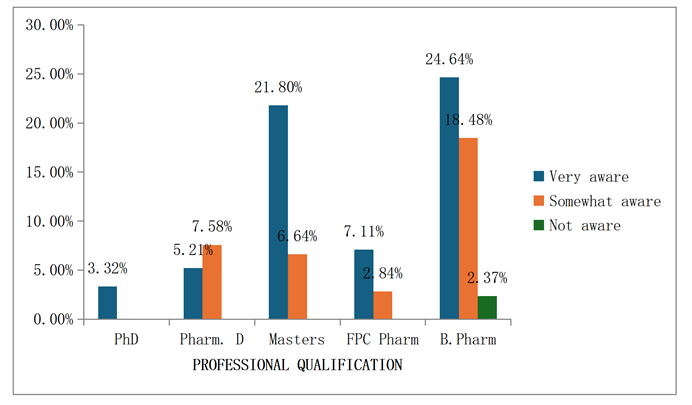
Figure 14: Relationship between Professional Qualification and Awareness on Creating a Judgement-Free Environment for Interaction
More than half of participants across all groups of professional qualification agree they can identify signs of intimate partner violence /abuse and reporting it where necessary. However, a lower percentage of respondents across some groups disagree. These include 5.21 % B. Pharm, 3.32 % Masters, 1.90 % Pharm. D.

Figure 15: Relationship between Professional Qualification and Ability to Identify and Report Abuse
Attitude
Measuring Relationship between Attitude and Gender
In addition to the descriptive statistical analysis, a crosstab analysis was carried out using Chi-square test to determine association between the attitude of the respondents and their respective gender. Below are questions asked and responses by pharmacists.
Question: Nursing mothers need "extra" care from their intimate partners during the postnatal period: Results showed that more than half of the respondents 82 Females, 91 Males of agree that nursing mothers need "extra" care from their intimate partners during the postnatal period. These results were statistically significant with p-value = 0.000 and 0.0345 at 5 % alpha and chi- square value of 0.687 and 4.345.
Question: I have adequate persuasive skills to encourage unwilling intimate partners to provide support to their female partners during the postpartum period: More than half of the population agree that they have adequate persuasive skills to encourage unwilling intimate partners to provide support to their female partners during the postpartum period. More males (75) and less females (59) tend to agree. These results were statistically significant with p-value = 0.005 and 0.004 at 5% alpha and chi- square value of 10.737 and 10.923.
Question: I need additional training to counsel and encourage intimate partners on the need for family planning and the need to abstain from sexual intercourse during the first six weeks postpartum, as recommended: 84 women and 4 men agree that they need additional training to counsel and encourage intimate partners on the need for family planning and the need to abstain from sexual intercourse during the first six weeks postpartum, as recommended. These results were statistically significant with p-value = 0.097 and 0.049 at 5% alpha and chi-square value of 6.316 and 7.889. female pharmacists tend to perceive encouraging male partners as a challenge. More male pharmacists believe they can have adequate training to counsel and persuade their male counterparts to be involved in care.
Question: I am competent to provide pharmaceutical care in delivering postpartum care: More than half of the population agree that they are competent to provide pharmaceutical care in delivering postpartum care. The results were statistically significant with p-value = 0.001 and 0.062 at 5% alpha and chi-square value of 4.095 and 8.342.
Question: I need additional training to interact, counsel and persuade intimate partners to get involved with delivering care for their postpartum partner and child: Although a huge number of the population believe they are competent to provide pharmaceutical care, the same population agree that they need additional training to interact, counsel and persuade intimate partners to get involved with delivering care for their postpartum partner and child. These results were statistically significant with p-value = 0.008 and 0.001 at 5% alpha and chi-square value of 11.865 and 16.114.
|
Statements |
Gender |
Agree |
Disagree |
Neutral |
X2 |
p-value |
|
Nursing mothers need "extra" care from their intimate partners during the postnatal period |
Female |
82 |
6 |
11 |
0.687 |
0.0000 |
|
Male |
91 |
5 |
6 |
4.345 |
0.0345 |
|
|
I am willing to encourage unwilling intimate partners to provide support to their female partners during the postpartum period |
Female |
59 |
9 |
31 |
10.737 |
0.005 |
|
Male |
75 |
21 |
16 |
10.923 |
0.004 |
|
|
I need additional training to counsel and encourage intimate partners on the need for family planning and the need to abstain from sexual intercourse during the first six weeks postpartum, as recommended |
Female |
84 |
8 |
7 |
6.316 |
0.097 |
|
Male |
4 |
89 |
15 |
7.889 |
0.049 |
|
|
I need additional training to interact, counsel and persuade intimate partners to get involved with delivering care for their postpartum partner and child |
Female |
96 |
0 |
3 |
11.865 |
0.008 |
|
Male |
98 |
7 |
7 |
16.114 |
0.001 |
|
|
I am competent to provide pharmaceutical care in delivering postpartum care |
Female |
96 |
3 |
16 |
4.095 |
0.001 |
|
Male |
72 |
16 |
8 |
8.342 |
0.062 |
Table 2: Measure of the Level of Relationship between Attitude and Gender
Table 3.3 shows a crosstabulation of the association between the attitude of the respondents and their respective years of experience using a chi-square test. Below are questions asked and responses by pharmacists.
Question: Nursing mothers need "extra" care from their intimate partners during the postnatal period: More than half of the entire population agree that nursing mothers need "extra" care from their intimate partners during the postnatal period with 57 from less than 5 group, 60 from 5 to 10 group, 82 from 11 to 20 group and all 6 members of the 21 and above group. These results were statistically significant with p-values 0.0000, 0.0345, 0.354 at 5% alpha and chi-square values of 0.687.4.345 from groups 11 to 20 and 21 and above respectively.
Question: I have adequate persuasive skills to encourage unwilling intimate partners to provide support to their female partners during the postpartum period: In this context, 59 pharmacists from less than 5 group, 61 from 5 to 10 group, 70 from 11 to 20 group and 80 from 21 and above group agree that they have adequate persuasive skills to encourage unwilling intimate partners to provide support to their female partners during the postpartum period. This forms more than half of the entire population. These results were statistically significant with p-values 0.008 and 0.0000 at 5% alpha and chi-square values of 7.864 and 0.127 for groups 11 to 20 and 21 and above.
Question: I am competent to provide pharmaceutical care in delivering postpartum care: More than half of the population agree that they are competent to provide pharmaceutical care in delivering postpartum care. Majority of respondents who agree were those with less than 5 years of work experience. The results were statistically significant with p-value = 0.0000 at 5% alpha and chi-square value of 0.127.
Question: I need additional training to interact, counsel and persuade intimate partners to get involved with delivering care for their postpartum partner and child: Out of 211 respondents, 194 pharmacists agree that they need additional training on interpersonal and persuasion skills in the context of male inclusion in pharmaceutical care. Across all groups, 194 pharmacists agree, 7 pharmacists disagree, and 10 pharmacists were neutral, neither agreeing nor disagreeing. These results were statistically significant with p-values 0.008, 0.001, 0.038 at 5% alpha and chi- square values of 11.865, 16.114, 0.038 for groups less than 5, 5 to 10, 21 and above respectively.
Question: I need additional training to counsel and encourage intimate partners on the need for family planning and the need to abstain from sexual intercourse during the first six weeks postpartum, as recommended: More than half of the population agree that they need additional training to counsel and encourage intimate partners on the need for family planning and the need to abstain from sexual intercourse during the first six weeks postpartum, as recommended. Across all groups, 177 pharmacists agree, 23 pharmacists disagree, and 11 pharmacists were neutral, neither agreeing nor disagreeing. These results were statistically significant with p-values 0.008, 0.001, 0.016, 0.035 at
5% alpha and chi-square values of 11.865, 19.114, 20.363, 17.780 respectively.
|
Statements |
Years of experience |
Agree |
Disagree |
Neutral |
X2 |
p-value |
|
Nursing mothers need "extra" care from their intimate partners during the postnatal period |
less than 5 |
57 |
3 |
1 |
3.396 |
0.334 |
|
5 to 10 |
60 |
0 |
1 |
4.532 |
0.209 |
|
|
11 to 20 |
82 |
1 |
0 |
0.687 |
0.0000 |
|
|
21 and above |
6 |
0 |
0 |
4.345 |
0.0345 |
|
|
I have adequate persuasive skills to encourage unwilling intimate partners to provide support to their female partners during the postpartum period |
less than 5 |
59 |
4 |
1 |
3.396 |
0.354 |
|
5 to 10 |
61 |
0 |
1 |
4.532 |
0.219 |
|
|
11 to 20 |
70 |
5 |
10 |
7.864 |
0.008 |
|
|
21 and above |
80 |
1 |
0 |
0.127 |
0.0000 |
|
|
I am competent to provide pharmaceutical care in delivering postpartum care |
less than 5 |
70 |
1 |
1 |
3.396 |
0.354 |
|
5 to 10 |
38 |
0 |
2 |
4.532 |
0.219 |
|
|
11 to 20 |
57 |
0 |
1 |
7.098 |
0.53 |
|
|
21 and above |
40 |
0 |
2 |
0.127 |
0.0000 |
|
|
I need additional training to interact, counsel and persuade intimate partners to get involved with delivering care for their postpartum partner and child. |
less than 5 |
54 |
3 |
3 |
11.865 |
0.008 |
|
5 to 10 |
52 |
4 |
4 |
16.114 |
0.001 |
|
|
11 to 20 |
82 |
0 |
3 |
8.342 |
0.062 |
|
|
21 and above |
6 |
0 |
0 |
17.780 |
0.038 |
|
|
I need additional training to counsel and encourage intimate partners on the need for family planning and the need to abstain from sexual intercourse during the first six weeks postpartum, as recommended |
less than 5 |
49 |
11 |
0 |
11.865 |
0.008 |
|
5 to 10 |
52 |
4 |
4 |
19.114 |
0.001 |
|
|
11 to 20 |
70 |
8 |
7 |
20.363 |
0.016 |
|
|
21 and above |
6 |
0 |
0 |
17.780 |
0.038 |
Table 3: A Measure of the Level of Relationship between Attitude and Years of Experience
Practice
Measuring the Relationship between Practice and Gender of Pharmacist
A crosstabulation using chi-square test to determine the relationship between practice and gender of pharmacist is shown in table 3.4. Below are questions asked and responses by pharmacists.
Question: At the point of pharmaceutical care delivery, I request the audience of intimate partners of nursing mothers: Only less than half of all female pharmacist respondents (34 out of 99) “always” request the audience of intimate partners of nursing mothers for counselling during PC. 20 of them “never”, and 45 ofthem “sometimes” request their audience for counselling. Out of112 male respondents, only 40% engage the male partners, 18 admit to “never” engage them and 54 indicate that they “sometimes” engage them. These results were statistically significant with p-values 0.025 at 5% alpha and chi-square value of 3.786.
Question: I allot adequate time to counsel intimate partners of nursing mothers on the need to be involved in mother care and childcare. (Childcare: baby feeding, bathing, diaper changing, pacification): 17 female pharmacists admit to “always” allotting adequate time to counsel male patients, 12 female pharmacists “never” with the other 70 pharmacists admitting to “sometimes”.
It is not very different for the male pharmacists who 35 admit to “always”, 15 admit to “never” and 62 admit to “sometimes”. These results are statistically significant with p-value 0.043 and 0.041 at 5% alpha and chi-square value of 6.272 and 6.379 respectively.
Question: I encourage intimate partners to provide support (including financial, physical, and psychological) to the nursing mothers: 67 out of 99 female pharmacists answered to “always” and 3 female pharmacists answered to “never”. For male pharmacists, 89 out of 105 answered to “never” and 4 answered to “always”. 29 female and 15 males answered “sometimes”. More female pharmacists than male tend to encourage intimate partners to provide financial, physical, and psychological support to nursing mothers. These results are statistically significant with p-values
0.055 and 0.029 at 5% alpha and chi-square value of 7.595 and
9.014 respectively.
Question: I am a practitioner of contraception counselling and encourage abstinence from sexual intercourse for a period of up to six weeks postpartum. I educate intimate partners of nursing mothers on condom use and proper disposal of condoms: For this statement, 77 female pharmacists and 72
male pharmacists answered “always”. A very negligible number answered to “never” on being practitioners of contraception and abstinence counselling. These results were statistically significant with p-values 0.001 and 0.032 at 5% alpha and chi-square values of 6.168 and 7.717 respectively.
Question: I ensure documentation of all pharmaceutical care activities: More than half the population; 67 male and 77 females ensure documentation of pharmaceutical care activities. These results are statistically significant with p-values 0.023 at 5% alpha and chi-square value of 8.342.
Question: I follow up on the intimate partners of postpartum women via SMS, phone calls, e-mails to ensure compliance with pharmacological and non- pharmacological therapy: Less than half of the pharmacists from both genders “always” do a follow up. Majority admitted to doing follow-ups “sometimes” with 65 pharmacists across both genders admitting to “never” doing a follow-up after postpartum care. These results are statistically significant with p-values 0.035 and 0.042 at 5% alpha and chi- square values of 3.370 and 4.140 respectively.
|
Statements |
Gender |
Always |
Never |
Sometimes |
x2 |
p-value |
|
At the point of pharmaceutical care delivery, I request the audience of intimate partners of nursing mothers |
female |
34 |
20 |
45 |
3.023 |
0.388 |
|
male |
40 |
18 |
54 |
3.786 |
0.025 |
|
|
I allot adequate time to counsel intimate partners of nursing mothers on the need to be involved in mother care and childcare. (Childcare: baby feeding, bathing, diaper changing, pacification) |
female |
17 |
12 |
70 |
6.272 |
0.043 |
|
male |
35 |
15 |
62 |
6.379 |
0.041 |
|
|
I encourage intimate partners to provide support (including financial, physical and psychological) to the nursing mothers. |
female |
67 |
3 |
29 |
7.595 |
0.055 |
|
male |
4 |
89 |
15 |
9.014 |
0.029 |
|
|
I am a practitioner of contraception counselling and encourage abstinence from sexual intercourse for a period of up to six weeks postpartum. I educate intimate partners of nursing mothers on condom use and proper disposal of condoms |
female |
77 |
5 |
17 |
6.168 |
0.001 |
|
male |
72 |
16 |
8 |
7.717 |
0.032 |
|
|
I encourage intimate partners to accompany the nursing mothers on subsequent clinic appointments |
female |
56 |
8 |
35 |
4.928 |
0.177 |
|
male |
51 |
15 |
46 |
5.720 |
0.126 |
|
|
I encourage intimate partners to ensure the nursing mothers' compliance to prescribed medication and lifestyle optimisation |
female |
77 |
5 |
17 |
6.168 |
0.104 |
|
male |
72 |
16 |
8 |
7.717 |
0.052 |
|
|
I ensure documentation of all pharmaceutical care activities |
female |
67 |
5 |
27 |
9.528 |
0.023 |
|
male |
77 |
10 |
25 |
8.342 |
0.062 |
|
|
I follow up on the intimate partners of postpartum women via SMS, phone calls, e-mails to ensure compliance with pharmacological and non- pharmacological therapy |
female |
16 |
33 |
50 |
3.370 |
0.035 |
|
male |
21 |
32 |
59 |
4.140 |
0.042 |
Table 4: A Measure of the Level of Relationship between Practice and Gender of Pharmacists
Below are questions asked about practice and responses by pharmacists.
Question: At the point of pharmaceutical care delivery, I request the audience of intimate partners of nursing mothers: An unusual low number of respondents were obtained for this statement with most of the respondents (72 out of 112) answering to “never” requesting the audience of intimate partners of nursing mothers for counselling during PC. Pharmacists (32) with 11 to 20 years’ experience formed most of this group. These results were statistically significant with p-values 0.0008,0.006,0.000,0.0345 at 5% alpha and chi-square value of 22.174,22.903, 0.687, 4.345 respectively.
Question: I allot adequate time to counsel intimate partners of nursing mothers on the need to be involved in mother care and childcare. (Childcare: baby feeding, bathing, diaper changing, pacification): Many pharmacists (93 out of) “always” allot adequate time to offer free counselling to men on the need to support nursing mothers. 102 pharmacists “sometimes” allot adequate time to offer free counselling. 16 pharmacists “never” set out time to counsel. Pharmacists with 11 to 20 years’ experience form a larger part of respondents who “always” and “sometimes” offer free counselling to men. These results are statistically significant with p-value 0.007, 0.007, 0.008, 0.0000 at 5% alpha
and chi-square value of 14.396, 17.703, 17.719, 0.197 respectively.
Question: I encourage intimate partners to provide support (including financial, physical, and psychological) to the nursing mothers: More than half of the respondents (135 out of 205) answered to “always” encouraging men to provide financial, physical, and psychological support to nursing mothers. 59 pharmacists out of 135 are from the 11 to 20 years of experience group. Likewise, out of the 56 pharmacists that answered “sometimes”, majority (22) are from the 11 to 20 years of experience group. Few pharmacists “never” encourage such support.
Question: I am a practitioner of contraception counselling and encourage abstinence from sexual intercourse for a period of up to six weeks postpartum. I educate intimate partners of nursing mothers on condom use and proper disposal of condoms: Out of 211 respondents, 110 answered “always” to this statement. 69 answered “sometimes” and 32 answered “never”. Pharmacists with 11 to 20 years’ experience formed majority of the groups that answered “always” and “sometimes” with a frequency of 50 and 23 respectively.
These results were statistically significant with p-values 0.008,0.001, 0.016, 0.038 at 5% alpha and chi-square values of 11.865, 19.114, 20.363, 17.780 respectively.
Question: I ensure documentation of all pharmaceutical care activities: Out of the 144 pharmacists that “always” document PC activities, 61 fall in the 11 to 20 years of experience group and form the majority. Similarly, 24 pharmacists out of the 52 that “sometimes” document PC activities are from the same 11 to 20. Years of experience group. 15 pharmacists across different years of experience groups “never” document PC activities. These results are statistically significant with p-values 0.002, 0.000, 0.087, 0.050 at 5% alpha and chi-square value of 46.002, 50.723, 40.009, 45.887 respectively.
Question: I follow up on the intimate partners of postpartum women via SMS, phone calls, e-mails to ensure compliance with pharmacological and non- pharmacological therapy: Less than half of the pharmacists across all groups “always” do a follow up. Majority (109) admitted to doing follow-ups “sometimes” with 65 pharmacists across all groups admitting to “never” doing a follow-up after postpartum care. These results are statistically significant with p-values 0.008, 0.001, 0.010 at 5% alpha and chi- square values of 21.480, 23.690 and 19.114 for groups less than 5, 5 to 10, 21 and above respectively.
|
Statements |
Years of experience |
Always |
Never |
Sometimes |
X2 |
p-value |
|
At the point of pharmaceutical care delivery, I request the audience of intimate partners of nursing mothers |
Less than 5 |
0 |
23 |
19 |
22.174 |
0.008 |
|
5 to 10 |
2 |
15 |
9 |
22.903 |
0.006 |
|
|
11 to 20 |
0 |
32 |
10 |
0.687 |
0.0000 |
|
|
21 and above |
0 |
2 |
0 |
4.345 |
0.0345 |
|
|
I allot adequate time to counsel intimate partners of nursing mothers on the need to be involved in mother care and childcare. (Childcare: baby feeding, bathing, diaper changing, pacification) |
Less than 5 |
59 |
4 |
1 |
14.396 |
0.007 |
|
5 to 10 |
10 |
4 |
46 |
17.703 |
0.007 |
|
|
11 to 20 |
22 |
8 |
51 |
17.719 |
0.008 |
|
|
21 and above |
2 |
0 |
4 |
0.197 |
0.0000 |
|
|
I encourage intimate partners to provide support (including financial, physical, and psychological) to the nursing mothers. |
Less than 5 |
36 |
6 |
18 |
7.802 |
0.354 |
|
5 to 10 |
40 |
4 |
16 |
10.062 |
0.219 |
|
|
11 to 20 |
59 |
4 |
22 |
7.098 |
0.53 |
|
|
21 and above |
0 |
6 |
0 |
0.127 |
0.554 |
|
|
I am a practitioner of contraception counselling and encourage abstinence from sexual intercourse for a period of up to six weeks postpartum. I educate intimate partners of nursing mothers on condom use and proper disposal of condoms |
Less than 5 |
20 |
9 |
31 |
11.865 |
0.008 |
|
5 to 10 |
37 |
10 |
13 |
19.114 |
0.001 |
|
|
11 to 20 |
50 |
12 |
23 |
20.363 |
0.016 |
|
|
21 and above |
3 |
1 |
2 |
17.780 |
0.038 |
|
|
I encourage intimate partners to accompany the nursing mothers on subsequent clinic appointments |
Less than 5 |
26 |
14 |
20 |
11.865 |
0.008 |
|
5 to 10 |
31 |
7 |
22 |
19.114 |
0.001 |
|
|
11 to 20 |
44 |
2 |
39 |
27.552 |
0.001 |
|
|
21 and above |
3 |
1 |
2 |
30.360 |
0.000 |
|
|
I encourage intimate partners to ensure the nursing mothers' compliance to prescribed medication and lifestyle optimisation |
Less than 5 |
36 |
6 |
18 |
28.342 |
0.001 |
|
5 to 10 |
53 |
5 |
2 |
38.136 |
0.000 |
|
|
11 to 20 |
60 |
0 |
25 |
34.675 |
0.980 |
|
|
21 and above |
6 |
0 |
0 |
40.654 |
0.991 |
|
|
I ensure documentation of all pharmaceutical care activities |
Less than 5 |
27 |
13 |
20 |
46.002 |
0.002 |
|
5 to 10 |
50 |
2 |
8 |
50.723 |
0.000 |
|
|
11 to 20 |
61 |
0 |
24 |
40.009 |
0.087 |
|
|
21 and above |
6 |
0 |
0 |
45.887 |
0.050 |
|
|
I follow up on the intimate partners of postpartum women via SMS, phone calls, e-mails to ensure compliance with pharmacological and non- pharmacological therapy |
Less than 5 |
8 |
28 |
24 |
21.480 |
0.008 |
|
5 to 10 |
14 |
11 |
35 |
23.690 |
0.001 |
|
|
11 to 20 |
15 |
26 |
44 |
20.096 |
0.986 |
|
|
21 and above |
0 |
0 |
6 |
19.114 |
0.010 |
Table 5: A Measure of the Level of Relationship between Practice and Years of Experience
Semi-structured Interviews
Tables 3.6 and 3.7 illustrate a summary of the collated themes derived from the collective responses of pharmacists during the interview sessions
|
Measure |
Codes |
Themes |
|
Suggestions for optimization of health and wellbeing of nursing mothers. |
support them to have some ‘me time’, take turns to pacify baby, put baby to sleep, encourage rest at intervals |
Encourage rest |
|
|
Proper dieting, improved diet, balanced diet for nursing mothers, address nutritional needs, feed well, proper nutrition, |
Encourage adequate diet |
|
|
Assist with domestic chores, assist with cooking, employ house help, employ nanny, physical support |
Domestic support |
|
|
Accompany to postnatal visits, vaccination, circumcision, ear piercing |
Encourage hospital visits |
|
|
Community awareness, hygiene education, male education, health talks |
Awareness/education of partners |
|
|
Healthy company, effective communication between couples, good time togetherness, date nights, |
Emotional support |
|
|
Paternity leave for fathers, laws to mandate male inclusion in care and postnatal counselling, subsidies and incentives, |
Policies |
|
|
Observe and report depression |
Suicide watch
|
|
Measure |
Codes |
Themes |
|
Challenges encountered by pharmacists in male inclusion for pharmaceutical care delivery |
Language barrier, traditions, beliefs, mindset, African patriarchal mindset, stigmatization |
Cultural/religious barriers |
|
|
Ignorance, lack of understanding |
Illiteracy/ignorance |
|
|
Unavailable partner, non-challant and uncooperative men, presence of other wives, unwillingness, reluctance, lack of interest, |
Apathy |
|
|
Busy partner, tight schedule, daily hustle, occupation |
Busy work schedule of men |
|
|
Ineffective communication between couples, psychological stress, Partners not living together, mindset, unwillingness, long distance relationships, secretive mothers, lack of cooperation |
Interpersonal factors between couples |
|
|
Lack of effective communication skills, interpersonal skills of pharmacists. |
Pharmacist-related factors |
Table 7: Responses Generated From Pharmacists on Challenges Encountered By Pharmacists during the Involvement of Men in Pharmaceutical Care Delivery
Discussion
Pharmacists across all age groups and professional qualifications tend to be aware of the benefits of involving intimate partners of nursing mothers during the provision of pharmaceutical care delivery.
The World Health Organisation (WHO) has made some recommendations for postnatal care, including the right timing of discharge from a medical facility after birth (after 24 hours for uncomplicated vaginal delivery), postnatal contacts after discharge, home visits after discharge, assessment of mother and child, exclusive breastfeeding, cord care, immunisation, bath and playtime with the baby, counselling of mother, iron and folic acid supplementation, prophylactic antibiotics, and psychosocial support. Evidence obtained affirms that pharmacists are aware of the WHO recommendations as best practices (WHO, 2013).
Pharmacists across all groups have adequate knowledge and information about the benefits of couple counselling, impact of intimate partner support on physical and mental health of nursing mothers, benefits of targeting men for health education and awareness programs on reproductive health, benefits of men accompanying their partners to follow-up and other MCH related activities, benefits of creating a judgement-free environment during counselling, adequate knowledge on family planning methods. Given their relationships with others, especially their partners and families, men need to be involved for them to: support family planning and contraception equally; share responsibility for promoting healthy sexuality and reproduction; enhance maternal, new-born, and child health; prevent mother-to-child HIV transmission; and promote sexual and reproductive rights for all (Shand and Marcell, 2021).
Higher percentage of comprehension obtained in pharmacists of the 36 to 45 years could be attributed to the higher frequency
of pharmacist respondents in the group. Higher percentage of comprehension obtained in pharmacists with B.Pharm qualification could be attributed to how individuals with B.Pharm qualification are more likely to have passed through pharmacy education recently. Thus, they are likely to be more knowledgeable on recent trends in pharmaceutical care.
Results obtained from KAP quantitative survey are in synergy with the themes generated from the qualitative data. Codes generated from pharmacists’ response on non-pharmacological measures that will be beneficial during inclusion of male partner support include domestic and emotional support from partners, partners to encourage and support hospital visits, partners to encourage and support rest and optimal diet, partner education.
The results from both data sets show that pharmacists have adequate knowledge on benefits of inclusion of male partners in pharmaceutical care delivery. This satisfies objective one of this study; to assess pharmacists’ perception of the benefits of inclusion of male partners in the pharmaceutical care plan process.
Regardless of gender and years of experience, pharmacists tend to have similar perceptions of the positive impact of male inclusion in pharmaceutical care delivery. The results show that a high percentage of pharmacists across both groups agree that nursing mothers need "extra" physical, psychological, emotional, and financial care from their intimate partners during the postnatal period. An almost equal number of pharmacists from both genders believe they are competent to provide adequate pharmaceutical care delivery in relation to male partner inclusion. Many pharmacists also believe they have adequate persuasive skills to involve men in care. However, more male pharmacists tend to be more confident of their ability to persuade men to be involved in care delivery than female pharmacists. A higher number of female than male pharmacists also tend to believe they need additional training to engage men in different aspects of the postnatal pharmaceutical care delivery.
Measuring perception of pharmacists based on years of experience shows that pharmacists across all groups have similar perceptions of the need to support nursing mothers during the postnatal period and their competence to deliver such care as pharmacists. Pharmacists generally believe they have adequate knowledge to persuade men to be involved in care. Majority of pharmacists across all groups also believe they need additional training in all aspects of pharmaceutical care related to postpartum care delivery.
Using the KAP quantitative survey, objective three explored pharmacists’ practice of male partner inclusion in postnatal pharmaceutical care delivery. Results from the KAP questionnaire showed that a higher proportion of pharmacists across all years of experience and gender groups are practitioners of male partner inclusion in pharmaceutical care delivery. Results indicate that while many pharmacists are practitioners of male inclusion at various stages of postnatal pharmaceutical care delivery, a significant number of pharmacists tend to neglect the practice. An exploration of pharmacists’ knowledge in objective one indicated that up to 90% of pharmacists are aware of the benefits of the practice of male inclusion in care. Despite this knowledge, a non- negligible number of pharmacists tend to overlook involving men during the postnatal care process.
Objective four (4) explored challenges encountered by pharmacists in the process of involving men in care provision for post-partum patients. Themes generated from pharmacists’ responses show that they encounter both patient-related and pharmacist-related problems. Patient-related problems outlined by pharmacists include ignorance of men on benefits of their involvement, apathy, or lack of interest of men, busy work schedule, cultural and religious barriers. Interpersonal relationship between couples was cited as a contributory factor to the challenges pharmacists encounter in engaging men. Men's actions, such as abuse or neglect, have a direct impact on their partner's and children's health. Men's active involvement in MCH has significant implications because of their enormous social and economic impact within the family (Bhatta, 2013). Some of these problems arise due to the African patriarchal system which inadvertently affects the awareness and willingness of men to be involved. In numerous places, the male patriarchal dynamics make it unusual to see men at prenatal clinics, and it is unfathomable to find males accompanying their partners during maternal and child health services (Demissie, Bulto, and Terfassa, 2016). Craymah, Oppong, and Tuoyire (2017) agree that traditionally, maternal health problems have been considered entirely a female concern and have been addressed as accordingly. As a result, men have often been barred access to MCH services, upholding the misconception that only women can become pregnant and giving birth. Some pharmacist-related problems identified were lack of effective communication and interpersonal skills which affects their ability to engage and persuade the male partners to get involved.
Finally, the challenges encountered by pharmacists as obtained from objective four (4) could serve as a plausible explanation for the lack of zeal of pharmacists to engage men in postnatal pharmaceutical care delivery, as highlighted in objective (3) three above. To enhance men's involvement in reproductive healthcare, reproductive health initiatives should concentrate on removing barriers to men's supportive behaviours (Roudsari, Sharifi and Goudarzi, 2023). The assumption by pharmacists that it will be difficult to persuade men to get involved is a barrier itself.
Men frequently act as healthcare's gatekeepers in LMICs. Most decisions that directly affect their partner's and kids' health are made by them. According to Ampt et al. (2015) and Yargawa and Leonardi-Bee (2015), their decisions have an impact on how resources are used, how people can access healthcare services, how people use contraception and decide when to have children, how readily available nutrient-rich food is, and how much work women must do. It has long been known that greater maternal and adolescent health arises from male involvement in RMNCH (reproductive, maternity, neonatal, and child health). However, according to Lusambili et al. (2021) many low- and middle-income nations implement male involvement initiatives inefficiently. At the 1994 International Conference on Population and Development (ICPD) in Cairo, which also acknowledged that men needed SRH and that their involvement was crucial, male involvement in reproductive health was recommended as one of the fundamental interventions to improve maternal health outcomes (Bishwajit et al., 2017, Omo- Aghoja, 2013, and WHO, 2018). To reduce any detrimental effects on the dynamics of a couple's relationship, programmes to enhance male involvement should be carefully planned and implemented (Lusambili et al., 2021).
Conclusion
The aim of the research has been fulfilled by identifying the knowledge, attitude, and practice of pharmacists in male partner inclusion for postnatal pharmaceutical care delivery.
Objective one assessed pharmacists’ perception of the benefits of inclusion of male partners in the pharmaceutical care plan process. Pharmacists, regardless of demography have adequate knowledge of pharmaceutical care delivery as it relates to male involvement in care.
Objective two evaluated the perception and attitude of pharmacists of their professional capability to provide adequate postnatal pharmaceutical care. Female pharmacists are skeptical about their abilities to persuade men to get involved in care. Female pharmacists are also more interested in receiving additional training and development to provide care.
Objective three explored the extent to which pharmacists involve male partners in delivering pharmaceutical care. Pharmacists are practitioners of male partner inclusion in pharmaceutical care delivery
Objective four explored the challenges faced by pharmacists in ensuring male involvement in the care process. Pharmacist cited several patient-related and pharmacists related challenges they faced during in involving intimate partners of nursing mothers in postnatal pharmaceutical care delivery.
Although a high percentage of pharmacists have adequate comprehension of the benefits of involving men in postnatal pharmaceutical care delivery, a worrisome number of pharmacists tend to neglect the practice. This is attributable to challenges encountered by pharmacists as they have either encountered or they foresee certain patient-related and pharmacist-related factors that affect their capability to provide care within the context.
The major limitation of the research was its limited generalizability. The mixed-method research requires a smaller sample size compared to quantitative-only studies. This may limit the generalizability of findings to larger populations.
Another limitation was the complexity of analyzing mixed-method data and successful integration of the findings from two different data sets to arrive at meaningful conclusions.
References
1. Abdullah, S. H., & Raman, S. (2000). Quantitative and qualitative research methods: Some strengths and weaknesses. The Asia Pacific Journal of Educators and Education (Formerly Known as Journal of Educators and Education), 17(1), 1-15.
2. Akibu, M., Tsegaye, W., Megersa, T., & Nurgi, S. (2018). Prevalence and determinants of complete postnatal care service utilization in northern Shoa, Ethiopia. Journal of pregnancy, 2018(1), 8625437.
3. Ampt, F., Mon, M. M., Than, K. K., Khin, M. M., Agius, P. A., Morgan, C., ... & Luchters, S. (2015). Correlates of male involvement in maternal and newborn health: a cross-sectional study of men in a peri-urban region of Myanmar. BMC pregnancy and childbirth, 15, 1-11.
4. Angore, B. N., Tufa, E. G., & Bisetegen, F. S. (2018). Determinants of postnatal care utilization in urban community among women in Debre Birhan Town, Northern Shewa, Ethiopia. Journal of Health, Population and Nutrition, 37, 1-9.
5. Ani, F., Abiodun, O., Sotunsa, J., Faturoti, O., Imaralu, J., & Olaleye, A. (2016). Demographic factors related to male involvement in reproductive health care services in Nigeria. The European Journal of Contraception & Reproductive Health Care, 21(1), 57-67.
6. August, F., Pembe, A. B., Mpembeni, R., Axemo, P., & Darj, E. (2016). Community health workers can improve male involvement in maternal health: evidence from rural Tanzania. Global health action, 9(1), 30064.
7. Bhatta, D. N. (2013). Involvement of males in antenatal care, birth preparedness, exclusive breast feeding and immunizations for children in Kathmandu, Nepal. BMC pregnancy and childbirth, 13, 1-7.
8. Bishwajit, G., Tang, S., Yaya, S., Ide, S., Fu, H., Wang, M., ... & Feng, Z. (2017). Factors associated with male involvement in reproductive care in Bangladesh. BMC Public Health, 17, 1-8.
9. Boetker-Smith, G. (2006). Social Research Methods. Qualitative Research Journal, 6(1), 105-111.
10. Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative research in sport, exercise and health, 11(4), 589-597.
11. Buccheri, R. K., & Sharifi, C. (2017). Critical appraisal tools and reporting guidelines for evidenceâ?based practice. Worldviews on Evidenceâ?Based Nursing, 14(6), 463-472.
12. Cannell, C. F., & Khan, R. L. (1968). Interviewing7 in G. Lindzey and A. Aronson.
13. Choy, L. T. (2014). The strengths and weaknesses of research methodology: Comparison and complimentary between qualitative and quantitative approaches. IOSR journal of humanities and social science, 19(4), 99-104.
14. Clouse, K., Schwartz, S., Van Rie, A., Bassett, J., Yende, N. and Pettifor, A., 2014. “What they wanted was to give birth; nothing else”: barriers to retention in option B+ HIV care among postpartum women in South Africa. Journal of acquired immune deficiency syndromes (1999), 67(1), p.e12.
15. Comrie-Thomson, L., Tokhi, M., Ampt, F., Portela, A., Chersich, M., Khanna, R., & Luchters, S. (2015). Challenging gender inequity through male involvement in maternal and newborn health: critical assessment of an emerging evidence base. Culture, health & sexuality, 17(sup2), 177-189.
16. Craymah, J. P., Oppong, R. K., & Tuoyire, D. A. (2017). Male involvement in maternal health care at Anomabo, Central Region, Ghana. International journal of reproductive medicine, 2017(1), 2929013.
17. Davis, J., Luchters, S., & Holmes, W. (2013). Men and maternal and newborn health. Briefing paper.
18. Davis, J., Vyankandondera, J., Luchters, S., Simon, D., & Holmes, W. (2016). Male involvement in reproductive, maternal and child health: a qualitative study of policymaker and practitioner perspectives in the Pacific. Reproductive health, 13, 1-11.
19. Dell’olio, L., Ibeas, A., De Oña, J., & De Oña, R. (2018). Designing a survey for public transport users. Public Transp. Qual. Serv, 49-61.
20. Demissie, D. B., Bulto, G. A., Terfassa, T. G. (2016). Involvement of male in antenatal care, birth preparedness and complication readinessand associated factors in Ambo town, Ethiopia. J Health Med Nurs, 27(5), 14-23.
21. Ditekemena, J., Koole, O., Engmann, C., Matendo, R., Tshefu, A., Ryder, R., & Colebunders, R. (2012). Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reproductive health, 9, 1-8.
22. Dworkin, S. L. (2012). Sample size policy for qualitative studies using in-depth interviews. Archives of sexual behavior, 41, 1319-1320.
23. Elnour, A. A., El Mugammar, I. T., Jaber, T., Revel, T., & McElnay, J. C. (2008). Pharmaceutical care of patients with gestational diabetes mellitus. Journal of Evaluation in Clinical Practice, 14(1), 131-140.
24. Etikan, I., Musa, S. A., & Alkassim, R. S. (2016). Comparison of convenience sampling and purposive sampling. American journal of theoretical and applied statistics, 5(1), 1-4.
25. Greenspan, J. A., Chebet, J. J., Mpembeni, R., Mosha, I., Mpunga, M., Winch, P. J., ... & McMahon, S. A. (2019). Men’s roles in care seeking for maternal and newborn health: a qualitative study applying the three delays model to male involvement in Morogoro Region, Tanzania. BMC pregnancy and childbirth, 19, 1-12.
26. Hammond, R. W., Boyce, B., Briceland, L., Canaday, B., Carr-Lopez, S. M., Eggleston, S. T., ... & Yan, J. (2003). ASHP guidelines on documenting pharmaceutical care in patient medical records. American Journal of Health-System Pharmacy, 60(7), 705-707.
27. Hausmann-Mueala, S., Muela Ribera, J., & Nyamongo, I. (2003). Health-seeking behaviour and the health system response. Disease Control Priorities Project (DCPP). Working Paper. Langwick, SA Bodies, Politics, and African Healing: The matter of maladies in Tanzania.
28. Heale, R., & Forbes, D. (2013). Understanding triangulation in research. Evidence-based nursing, 16(4), 98-98.
29. Hepler, C. D., & Strand, L. M. (1990). Opportunities and responsibilities in pharmaceutical care. American journal of hospital pharmacy, 47(3), 533-543.
30. Hong, Q. N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., ... & Pluye, P. (2018). The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for information, 34(4), 285-291.
31. Iliyasu, Z., Abubakar, I. S., Galadanci, H. S., & Aliyu, M. H. (2010). Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. African journal of reproductive health, 14(1).
32. UNFPA, I. (2017). Global sexual and reproductive health service package for men and adolescent boys. London: IPPF and New York City: UNFPA, 7-11.
33. Jalal, S. M., Akhter, F., Abdelhafez, A. I., & Alrajeh, A. M. (2021, June). Assessment of knowledge, practice and attitude about biomedical waste management among healthcare professionals during COVID-19 crises in Al-Ahsa. In Healthcare (Vol. 9, No. 6, p. 747). MDPI.
34. Jamshed, S. (2014). Qualitative research method-interviewing and observation. Journal of basic and clinical pharmacy, 5(4), 87.
35. Jason, L., & Glenwick, D. (Eds.). (2016). Handbook of methodological approaches to community-based research: Qualitative, quantitative, and mixed methods. Oxford university press.
36. Johnson, R. B., & Christensen, L. B. (2024). Educational research: Quantitative, qualitative, and mixed approaches. Sage publications.
37. Kesmodel, U. S. (2018). Crossâ?sectional studies–what are they good for?. Acta obstetricia et gynecologica Scandinavica, 97(4), 388-393.
38. Kingsley, J. Y., Townsend, M., & Hendersonâ?Wilson, C. (2009). Cultivating health and wellbeing: members' perceptions of the health benefits of a Port Melbourne community garden. Leisure studies, 28(2), 207-219.
39. Krueger, R. A. (2014). Focus groups: A practical guide for applied research. Sage publications.
40. Launiala, A. (2009). How much can a KAP survey tell us about people's knowledge, attitudes and practices? Some observations from medical anthropology research on malaria in pregnancy in Malawi. Anthropology Matters, 11(1).
41. Ampt, F., Mon, M. M., Than, K. K., Khin, M. M., Agius, P. A., Morgan, C., ... & Luchters, S. (2015). Correlates of male involvement in maternal and newborn health: a cross-sectional study of men in a peri-urban region of Myanmar. BMC pregnancy and childbirth, 15, 1-11.
42. Luchters, S., Davis, J., Morgan, C., Agius, P.A., Khin, M.M., Than, K.K., Mon, M.M. and Ampt, F., 2015. Correlates of male involvement in maternal and newborn health: a cross- sectional study of men in a peri-urban region of Myanmar.
43. Maluka, S. O., & Peneza, A. K. (2018). Perceptions on male involvement in pregnancy and childbirth in Masasi District, Tanzania: a qualitative study. Reproductive health, 15, 1-7.
44. Mepham, S., Zondi, Z., Mbuyazi, A., Mkhwanazi, N., & Newell, M. L. (2011). Challenges in PMTCT antiretroviral adherence in northern KwaZulu-Natal, South Africa. AIDS care, 23(6), 741-747.
45. Nanjala, M., & Wamalwa, D. (2012). Determinants of male partner involvement in promoting deliveries by skilled attendants in Busia, Kenya. Global journal of health science, 4(2), 60.
46. Neale, J., & Strang, J. (2015). Blending qualitative and quantitative research methods to optimize patient reported outcome measures (PROMs). Addiction, 110(8), 1215-1216.
47. Nolan, M. T., & Mock, V. (Eds.). (2000). Measuring patient outcomes. Sage.
48. Ochieng, P. A. (2009). An analysis of the strengths and limitation of qualitative and quantitative research paradigms. Problems of Education in the 21st Century, 13, 13.
49. Ogugua, J.O., Amlogu, A.M., Aguiyi-Ikeanyi, C.N. and Udezi, A.W., 2023. Evaluation of Telepharmacy Services in Community Pharmacies in Abuja, Nigeria. Archives of Infect Diseases & Therapy, 7(1), pp.27-33.
50. Omo-Aghoja, L. (2013). Sexual and reproductive health: Concepts and current status among Nigerians. Afr J Med Health Sci, 12(2).
51. Ope, B. W. (2020). Reducing maternal mortality in Nigeria: addressing maternal health services’ perception and experience. Journal of Global Health Reports, 4, e2020028.
52. Roudsari, R. L., Sharifi, F., & Goudarzi, F. (2023). Barriers to the participation of men in reproductive health care: a systematic review and meta-synthesis. BMC Public Health, 23(1), 818.
53. Shand, T., & Marcell, A. V. (2021). Engaging men in sexual and reproductive health. In Oxford Research Encyclopedia of Global Public Health.
54. Singh, S., & Wassenaar, D. R. (2016). Contextualising the role of the gatekeeper in social science research. South African Journal of Bioethics and Law, 9(1), 42-46.
55. St Clair, R. (2017). Investigating the impact and potential of urban agriculture in the UK: observations from an institution- led initiative in Wythenshawe, South Manchester (Doctoral dissertation).
56. Sully, E. A., Biddlecom, A., Darroch, J. E., Riley, T., Ashford, L. S., Lince-Deroche, N., ... & Murro, R. (2020). Adding it up: investing in sexual and reproductive health 2019.
57. Taylor, E. and Hignett, S., 2014. Evaluating evidence: defining levels and quality using critical appraisal mixed methods tools. HERD: Health Environments Research & Design Journal, 7(3), pp.144-151.
58. Taylor, S. J., Bogdan, R., & DeVault, M. L. (2015). Introduction to qualitative research methods: A guidebook and resource. John Wiley & Sons.
59. Thomas, D. (Ed.). (2018). Clinical pharmacy education, practice and research: clinical pharmacy, drug information, pharmacovigilance, pharmacoeconomics and clinical research. Elsevier.
60. Tumuhamye, N., Rutebemberwa, E., Kwesiga, D., Bagonza, J., & Mukose, A. (2013). Client satisfaction with integrated community case management program in Wakiso District, Uganda, October 2012: A cross sectional survey. Health, 5(11), 1889-1898.
61. van den Berg, W., Brittain, K., Mercer, G., Peacock, D., Stinson, K., Janson, H., & Dubula, V. (2015). Improving men’s participation in preventing mother-to-child transmission of HIV as a maternal, neonatal, and child health priority in South Africa. PLoS medicine, 12(4), e1001811.
62. Wakui, N., Kikuchi, M., Ebizuka, R., Yanagiya, T., Togawa, C., Matsuoka, R., ... & Kato, H. (2022). Survey of Pharmacists’ Knowledge, Attitudes, and Practices (KAP) concerning COVID-19 Infection Control after Being Involved in Vaccine Preparation: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(15), 9035.
63. Wilson, C. (2014). Semi-structured interviews. Interview techniques for UX practitioners, 1, 23-41.
64. Wilson, V. (2012). Research methods: interviews.
65. World Health Organization. (2007). Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA, and the World Bank. In Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA, and The World Bank.
66. Advocacy, W. H. O. (2008). communication and social mobilization for TB control: a guide to developing knowledge, attitude and practice surveys. World Health Organization.
67. World Health Organization, 2008. Advocacy, communication and social mobilization for TB control: a guide to developing knowledge, attitude and practice surveys (No. WHO/HTM/ STB/2008.46). World Health Organization.
68. World Health Organization. (2012). Trends in maternal mortality: 1990 to 2010: WHO, UNICEF, UNFPA and The World Bank estimates. Trends in maternal mortality: 1990 to 2010: WHO, UNICEF, UNFPA and The World Bank estimates.
69. World Health Organization. (2018). WHO recommendations on intrapartum care for a positive childbirth experience. World Health Organization.
70. Yargawa, J., & Leonardi-Bee, J. (2015). Male involvement and maternal health outcomes: systematic review and meta- analysis. J Epidemiol Community Health, 69(6), 604-612.



